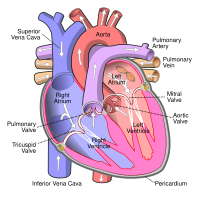
Photo from wikipedia
Cardiomyocytes exit the cell cycle and become terminally differentiated soon after birth. Therefore, in the adult heart, instead of an increase in cardiomyocyte number, individual cardiomyocytes increase in size, and… Click to show full abstract
Cardiomyocytes exit the cell cycle and become terminally differentiated soon after birth. Therefore, in the adult heart, instead of an increase in cardiomyocyte number, individual cardiomyocytes increase in size, and the heart develops hypertrophy to reduce ventricular wall stress and maintain function and efficiency in response to an increased workload. There are two types of hypertrophy: physiological and pathological. Hypertrophy initially develops as an adaptive response to physiological and pathological stimuli, but pathological hypertrophy generally progresses to heart failure. Each form of hypertrophy is regulated by distinct cellular signalling pathways. In the past decade, a growing number of studies have suggested that previously unrecognized mechanisms, including cellular metabolism, proliferation, non-coding RNAs, immune responses, translational regulation, and epigenetic modifications, positively or negatively regulate cardiac hypertrophy. In this Review, we summarize the underlying molecular mechanisms of physiological and pathological hypertrophy, with a particular emphasis on the role of metabolic remodelling in both forms of cardiac hypertrophy, and we discuss how the current knowledge on cardiac hypertrophy can be applied to develop novel therapeutic strategies to prevent or reverse pathological hypertrophy.Adult cardiac hypertrophy initially develops as an adaptive response to an increased workload, but this physiological growth can ultimately lead to pathological hypertrophy and disease. In this Review, Nakamura and Sadoshima summarize the characteristics and underlying mechanisms of physiological and pathological hypertrophy, and discuss possible therapeutic strategies targeting these pathways to prevent or reverse pathological hypertrophy.Key pointsThe heart initially undergoes hypertrophy in response to haemodynamic overload to increase contractility and reduce ventricular wall stress, but this adaptive hypertrophy transitions to heart failure through pathological remodelling.There are two types of hypertrophy, physiological and pathological, which differ in their underlying molecular mechanisms, cardiac phenotype, and prognosis.The type of hypertrophic stimuli and the nature of the downstream signalling mechanisms largely determine the fate of cardiac hypertrophy, which is either physiological or pathological.Prioritizing the regulators of pathological hypertrophy on the basis of their clinical relevance for therapeutic targeting is important to improve the outcomes in patients with pathological hypertrophy and heart failure.
Journal Title: Nature Reviews Cardiology
Year Published: 2018
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!