Photo from wikipedia
Background: severe carotid artery stenosis is a major cause of ischemic stroke and consequent neurological deficits. The most important steps of atherosclerotic plaque development, leading to carotid stenosis, are well-known;… Click to show full abstract
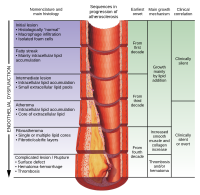
Background: severe carotid artery stenosis is a major cause of ischemic stroke and consequent neurological deficits. The most important steps of atherosclerotic plaque development, leading to carotid stenosis, are well-known; however, their exact timeline and intricate causal relationships need to be more characterized. Methods: in a cohort of 119 patients, who underwent carotid endarterectomy, we studied the histological correlations between arterial calcification patterns and localization, the presence of the inflammatory infiltrate and osteopontin expression, with ulceration, thrombosis, and intra-plaque hemorrhage, as direct signs of vulnerability. Results: in patients with an inflammatory infiltrate, aphasia was more prevalent, and microcalcification, superficial calcification, and high-grade osteopontin expression were characteristic. Higher osteopontin expression was also correlated with the presence of a lipid core. Inflammation and microcalcification were significantly associated with plaque ulceration in logistic regression models; furthermore, ulceration and the inflammatory infiltrate were significant determinants of atherothrombosis. Conclusion: our results bring histological evidence for the critically important role of microcalcification and inflammatory cell invasion in the formation and destabilization of advanced carotid plaques. In addition, as a calcification organizer, high-grade osteopontin expression is associated with ulceration, the presence of a large lipid core, and may also have an intrinsic role in plaque progression.
Journal Title: Biomedicines
Year Published: 2023
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!