Photo from wikipedia
Simple Summary Trabectedin and lurbinectedin are two potent onco-therapeutic drugs for the treatment of advanced soft tissue sarcomas. Here we show that, in addition to cancer cells, these molecules exert… Click to show full abstract
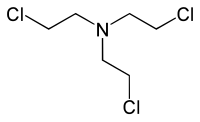
Simple Summary Trabectedin and lurbinectedin are two potent onco-therapeutic drugs for the treatment of advanced soft tissue sarcomas. Here we show that, in addition to cancer cells, these molecules exert important effects on macrophages and tissue-associated macrophages altering metabolic functions, such as respiration and cell viability. Interestingly, the macrophages from one-fourth of healthy individuals exhibit apoptotic cell death when treated with these drugs at therapeutic doses. These data are relevant to understand the action of these molecules in the context of chemotherapy of oncologic patients. Abstract Background: Tumor-associated macrophages (TAMs) play a crucial role in suppressing the immunosurveillance function of the immune system that prevents tumor growth. Indeed, macrophages can also be targeted by different chemotherapeutic agents improving the action over immune checkpoints to fight cancer. Here we describe the effect of trabectedin and lurbinectedin on human macrophage cell viability and function. Methods: Blood monocytes from healthy donors were differentiated into macrophages and exposed to different stimuli promoting functional polarization and differentiation into tumor-associated macrophages. Cells were challenged with the chemotherapeutic drugs and the effects on cell viability and function were analyzed. Results: Human macrophages exhibit at least two different profiles in response to these drugs. One-fourth of the blood donors assayed (164 individuals) were extremely sensitive to trabectedin and lurbinectedin, which promoted apoptotic cell death. Macrophages from other individuals retained viability but responded to the drugs increasing reactive oxygen production and showing a rapid intracellular calcium rise and a loss of mitochondrial oxygen consumption. Cell-membrane exposure of programmed-death ligand 1 (PD-L1) significantly decreased after treatment with therapeutic doses of these drugs, including changes in the gene expression profile of hypoxia-inducible factor 1 alpha (HIF-1α)-dependent genes, among other. Conclusions: The results provide evidence of additional onco-therapeutic actions for these drugs.
Journal Title: Cancers
Year Published: 2020
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!