Photo from wikipedia
Importance Sodium-glucose cotransporter 2 inhibitors, such as dapagliflozin, promote renal glucose excretion and reduce cardiovascular (CV) deaths and hospitalizations for heart failure (HHF) among patients with type 2 diabetes. The… Click to show full abstract
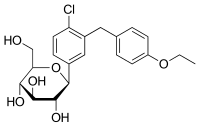
Importance Sodium-glucose cotransporter 2 inhibitors, such as dapagliflozin, promote renal glucose excretion and reduce cardiovascular (CV) deaths and hospitalizations for heart failure (HHF) among patients with type 2 diabetes. The relative CV efficacy and safety of dapagliflozin according to baseline kidney function and albuminuria status are unknown. Objective To assess the CV efficacy and safety of dapagliflozin according to baseline estimated glomerular filtration rate (eGFR) and urinary albumin to creatinine ratio (UACR). Design, Setting, and Participants This secondary analysis of the randomized clinical trial Dapagliflozin Effect on Cardiovascular Events-Thrombolysis in Myocardial Infarction 58 compared dapagliflozin vs placebo in 17 160 patients with type 2 diabetes and a baseline creatinine clearance of 60 mL/min or higher. Patients were categorized according to prespecified subgroups of baseline eGFR (<60 vs ≥60 mL/min/1.73 m2), urinary albumin to creatinine ratio (UACR; <30 vs ≥30 mg/g), and of chronic kidney disease (CKD) markers using these subgroups (0, 1, or 2). The study was conducted from May 2013 to September 2018. Interventions Dapagliflozin vs placebo. Main Outcomes and Measures The dual primary end points were major adverse cardiovascular events (myocardial infarction, stroke, and CV death) and the composite of CV death or HHF. Results At baseline, 1265 patients (7.4%) had an eGFR below 60 mL/min/1.73 m2, and 5199 patients (30.9%) had albuminuria. Among patients having data for both eGFR and UACR, 10 958 patients (65.1%) had an eGFR equal to or higher than 60 mL/min/1.73 m2 and an UACR below 30 mg/g (mean [SD] age, 63.7 [6.7] years; 40.1% women), 5336 patients (31.7%) had either an eGFR below 60 mL/min/1.73 m2 or albuminuria (mean [SD] age, 64.1 [7.1] years; 32.6% women), and 548 patients (3.3%) had both (mean [SD] age, 66.8 [6.9] years; 30.5% women). In the placebo group, patients with more CKD markers had higher event rates at 4 years as assessed using the Kaplan-Meier approach for the composite of CV death or HHF (3.9% for 0 markers, 8.3% for 1 marker, and 17.4% for 2 markers) and major adverse cardiovascular events (7.5% for 0 markers, 11.6% for 1 marker, and 18.9% for 2 markers). Estimates for relative risk reductions for the composite of CV death or HHF and for major adverse cardiovascular events were generally consistent across subgroups (both P > .24 for interaction), although greater absolute risk reductions were observed with more markers of CKD. The absolute risk difference for the composite of CV death or HHF was greater for patients with more markers of CKD (0 markers, -0.5%; 1 marker, -1.0%; and 2 markers, -8.3%; P = .02 for interaction). The numbers of amputations, cases of diabetic ketoacidosis, fractures, and major hypoglycemic events were balanced or numerically lower with dapagliflozin compared with placebo for patients with an eGFR below 60 mL/min/1.73 m2 and an UACR of 30 mg/g or higher. Conclusions and Relevance The effect of dapagliflozin on the relative risk for CV events was consistent across eGFR and UACR groups, with the greatest absolute benefit for the composite of CV death or HHF observed among patients with both reduced eGFR and albuminuria. Trial Registration ClinicalTrials.gov Identifier: NCT01730534.
Journal Title: JAMA cardiology
Year Published: 2021
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!