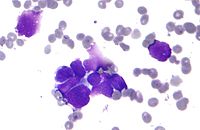
Photo from wikipedia
Importance Sex-associated differences in immune response are known, but a meta-analysis suggested men, compared with women, derive greater value from immunotherapy for advanced solid-organ malignant neoplasms. However, methodologic concerns and… Click to show full abstract
Importance Sex-associated differences in immune response are known, but a meta-analysis suggested men, compared with women, derive greater value from immunotherapy for advanced solid-organ malignant neoplasms. However, methodologic concerns and subsequent trials have placed these results in doubt. Objective To perform an updated, comprehensive meta-analysis that assesses the efficacy of immunotherapy in advanced cancers according to patient sex. Design, Setting, and Participants A systematic review of studies (n = 23) indexed in MEDLINE (PubMed), Embase, and Scopus from inception of these databases to October 2, 2018, was conducted. Randomized clinical trials that compared immunotherapy with standard of care in the treatment of advanced solid-organ malignant neoplasms were included if overall survival was reported as an outcome and if data stratified by patient sex were available. Observational studies, editorials, commentaries, review articles, non–peer-reviewed publications, studies that compared various immunotherapy regimens, studies that reported other measures of oncologic response, and studies that reported subgroup analyses for 1 sex only were excluded. Main Outcomes and Measures Overall survival, with a test for heterogeneity between women and men, to assess the null hypothesis that no difference in the survival advantage of immunotherapy exists by patient sex. Results This meta-analysis included 23 randomized clinical trials that reported on 9322 men (67.9%) and 4399 women (32.1%); the age of most patients was in the 70s. An overall survival benefit of immunotherapy was found for both men (hazard ratio [HR], 0.75; 95% CI, 0.69-0.81; P < .001) and women (HR, 0.77; 95% CI, 0.67-0.88; P = .002). Random-effects meta-analysis of study-level differences in response to immunotherapy demonstrated no statistically significant difference between the sexes (I2 = 38%; P = .60). Subgroup analyses according to disease site, line of therapy, class of immunotherapy, study methodology, and representation of women recapitulated these findings. Conclusions and Relevance Stratified analyses demonstrated no statistically significant association of patient sex with the efficacy of immunotherapy in the treatment of advanced cancers using overall survival as the outcome.
Journal Title: JAMA Oncology
Year Published: 2019
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!