Photo from wikipedia
Abstract Objectives Occupational physical loading has been reported to be associated with intervertebral disc degeneration. However, previous literature reports inconsistent results for different vertebral levels. The aim of our study… Click to show full abstract
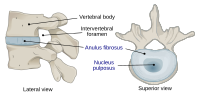
Abstract Objectives Occupational physical loading has been reported to be associated with intervertebral disc degeneration. However, previous literature reports inconsistent results for different vertebral levels. The aim of our study was to investigate the association between lumbar disc degeneration (LDD) at different vertebral levels and the self‐reported physical loading of occupation. Methods The study population consisted of 1,022 postmenopausal women and was based on the prospective Kuopio Osteoporosis Risk Factor and Prevention (OSTPRE) study cohort. The severity of LDD was graded from T2‐weighted MRI images using the five‐grade Pfirrmann classification. Five intervertebral levels (L1–L2 to L5–S1) were studied (total 5110 discs). The self‐rated occupational physical loading contained four groups: sedentary, light, moderate, and heavy. Results The heavy occupational physical loading group had higher odds for severe LDD at the L5–S1 vertebral level (OR 1.86, 95% CI: 1.19–2.92, p = .006) in comparison with the sedentary work group. A clear trend of increasing disc degeneration with heavier occupational loading was also observed at the L5–S1 level. Age, smoking, and higher body mass index (BMI) were associated with more severe LDD. Leisure‐time physical activity at the age of 11–17 years was associated with less severe LDD. Controlling for confounding factors did not alter the results. Conclusions There appears to be an association between occupational physical loading and severe disc degeneration at the lower lumbar spine in postmenopausal women. Individuals in occupations with heavy physical loading may have an increased risk for work‐related disability due to more severe disc degeneration.
Journal Title: Journal of Occupational Health
Year Published: 2022
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!