Photo from wikipedia
In this issue of the American Journal of Hematology Munir et al reported the final results of up to 6 years follow-up of the randomized RESONATE study, comparing the first-in-class… Click to show full abstract
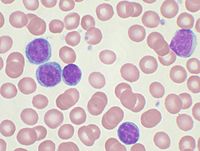
In this issue of the American Journal of Hematology Munir et al reported the final results of up to 6 years follow-up of the randomized RESONATE study, comparing the first-in-class Bruton Tirosin's kinase inhibitor (BTKi) ibrutinib, vs ofatumumab in patients with relapsed or refractory (r/r) chronic lymphocytic leukemia (CLL). Two previous reports described earlier results of this pivotal registration trial: the primary analysis and the latter one with median follow-up of 9.4 and 44 months, respectively. This final analysis, here reported, is highly relevant, as it adds two additional years of observation (median 65.3 months), for the 195 patients originally assigned to ibrutinib (median treatment duration 41 months). Data result in the longest follow-up for a cohort of CLL patients treated continuously with ibrutinib (exceeding also the recently published long-term update of the seminal PCYC 1102-1103 study). This observation time in the context of a well conducted randomized trial makes this report a treasure trove for defining efficacy and safety of ibrutinib in various CLL subgroups in the long term. Ibrutinib, together with PI3K inhibitor idelalisib, changed the treatment paradigm of B-cell neoplasms, switching from numbers of chemo-cycles to a continuous dosing of oral medication until progression or unacceptable toxicity. From the time of its full approval, ibrutinib largely replaced other options in r/r CLL, due to its efficacy especially in molecularly-defined high risk patients over chemoimmunotherapy regimens like BR or FCR, and a substantial superior tolerability profile over idelalisib-rituximab. Looking in details to RESONATE updated results, cumulative overall response rate (ORR) reached 91%, with a further slight increase of complete response (CR) rate up to 11%. At this mature time-point, median PFS remained impressively higher for ibrutinib compared to ofatumumab (44.1 vs 8.1 months). This happened even (44.1 vs 8.0 months) for patients with well-known genomic high-risk characteristics (del17p, TP53 mutation, del11q and/or unmutated IGHV status), which were enriched (82%) in this heavily pre-treated r/r CLL population. Dissecting PFS results according to different highrisk subgroups, a significantly lower PFS was observed in del17p and/or TP53 mutated patients (40.7 vs 56.9 months). Complex karyotype (CK) did not result associated with worse outcome. Notably, even in the PCYC-1102/1103 study, CK was not identified as an independent prognostic factor for PFS or OS, as survival in patients with CK was largely influenced by the coexistence of del17p. Unmutated IGHV prognostic value was completely overcome by ibrutinib as clearly illustrated by superimposable PFS curves, in line with other studies. Finally, patients with del11q experienced a noteworthy benefit with median PFS (60.7 months) exceeding the one of the whole ibrutinib cohort, consistent with a pooled analysis in about 600 patients. This fact qualifies ibrutinib as a precision medicine for this specific genomic subset of patients. The crude OS rate benefit is now reduced to only borderline significance, mainly as a result of the crossover effect to ibrutinib (68%) of patients originally randomized to ofatumumab. In fact, after adjusting for the crossover, ibrutinib arm retained significant OS benefit. Lastly, the rate of patients still on ibrutinib decreased to 22% (from 46% at 4 years), with disease progression (37%, including 10% of patients with evidence of Richter's transformation) and adverse events (AEs, 16%) being the major reasons of discontinuation. Richter's syndrome (RS) occurring during ibrutinib treatment warrants some special considerations. RESONATE population was heavily pre-treated (median three prior treatment lines) and more than half of patients carried TP53 mutation, which is one the most recurrent genetic risk factor for RS. Moreover, RS occurred early in the course of ibrutinib treatment: 8/20 occurring in the first and 10/20 during the second and third. This pattern parallels that of studies with novel agents in this setting, suggesting the presence of unrecognized transformation foci before treatment initiation. Richter's transformation events were reported also in idelalisib-rituximab (with apparent lower rate) and venetoclax-rituximab treated patients, as well. Type of treatments per se does not appear to affect the risk of RS, while the burden of previous treatment does. Received: 10 October 2019 Accepted: 12 October 2019
Journal Title: American Journal of Hematology
Year Published: 2019
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!