Photo from wikipedia
Chimeric antigen receptor T‐cell therapy (CAR T) is a novel intervention for relapsed/refractory diffuse large B‐cell lymphoma (R/R DLBCL) and other hematologic malignancies. However, it is associated with prolonged hematologic… Click to show full abstract
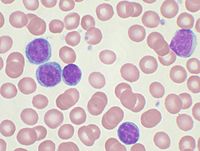
Chimeric antigen receptor T‐cell therapy (CAR T) is a novel intervention for relapsed/refractory diffuse large B‐cell lymphoma (R/R DLBCL) and other hematologic malignancies. However, it is associated with prolonged hematologic toxicity (PHT) that is unpredictable and can significantly impair patients' quality of life. Reported here is a single‐center experience with PHT in adult patients with R/R DLBCL who received commercial CAR T‐cell therapy between March 1, 2018 and May 30, 2020. Prolonged hematologic toxicity was defined as ≥ grade 3 neutropenia or thrombocytopenia at day +30 after CAR T‐cell therapy. Of the 31 patients identified, 18 patients (58%) developed PHT. Patients with PHT had a shorter 1‐year overall survival (OS) than patients without PHT (36% vs. 81%, P < .05). There were no differences in the median time to ANC recovery for those with PHT compared to patients without PHT (16 days vs. 15 days). Several risk factors were identified to be associated with PHT including CRS (P = .002), receipt of tocilizumab (P = .002) or steroids (P = .033), peak ferritin >5000 ng/ml (P = .048), peak C‐reactive protein (CRP) > 100 mg/L (P = .007), and ferritin greater than the upper limit of normal at day +30. Seven patients with PHT underwent a bone marrow biopsy after CAR T‐cell therapy; all showed complete aplasia or were hypocellular with cellularity ranging from <5% to 10%. These findings identify PHT as a significant toxicity associated with CAR T‐cell therapy and highlight the critical need for further investigations to describe PHT in larger cohorts and identify standards for management of this condition.
Journal Title: American Journal of Hematology
Year Published: 2021
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!