Photo from wikipedia
Since George A. Schumacher’s seminal contribution in 1965, accurate diagnosis of multiple sclerosis (MS) has relied on the detection of dissemination in time and dissemination in space (DIS). These criteria… Click to show full abstract
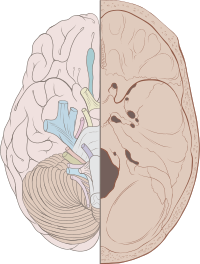
Since George A. Schumacher’s seminal contribution in 1965, accurate diagnosis of multiple sclerosis (MS) has relied on the detection of dissemination in time and dissemination in space (DIS). These criteria have not only withstood time, but have provided a conceptual framework integrating major methodological advances, for example, analysis of cerebrospinal fluid, evoked potentials, and imaging. Among the latter, magnetic resonance imaging (MRI) substantially transformed diagnostic procedures, as this technique provides unprecedented resolution for detection of asymptomatic or past inflammatory demyelinating events. As lesions discovered in the white matter are per se not specific for MS, meticulous characterization of lesion patterns by consortia such as the Magnetic Resonance Imaging in Multiple Sclerosis (MAGNIMS) group allowed the definition of MRI criteria, first incorporated in the 2001 MS diagnosis criteria by W. Ian McDonald et al and continuously refined during the subsequent revisions in 2005, 2010, and 2017. Despite this tremendous progress, it is remarkable that for the past and existing MS diagnosis criteria, the role of optic neuritis (ON) as “the archetypical first mode of presentation in multiple sclerosis” remained unclear. Although the MAGNIMS group initially suggested the inclusion of the optic nerve as a fifth predilection site for MRI-based lesion detection, additional to the (juxta)cortex, the periventricular white matter, the brainstem, and the spinal cord, a follow-up study was not able to corroborate this. Therefore, the International Panel on Diagnosis of Multiple Sclerosis judged that the evidence for DIS by purely MRI-dependent discovery of optic nerve lesions is not yet convincing but identified this issue as a high-priority area for further—mainly methodological—research. Visualization of optic nerve involvement by MRI requires dedicated magnetic resonance image acquisition approaches outperformed by specific optic nerve imaging by, for example, optical coherence tomography (OCT), with regard to sensitivity. However, OCT technology has been introduced to neurological practice only very recently, and systematic characterization of OCT-based detection of optic nerve damage in large cohorts of MS patients is lacking so far, as are standards for defining alterations of OCT parameters in health and MS. In the current issue, Nolan and colleagues from the International Multiple Sclerosis Visual System Consortium fill a substantial part of the research gap. Based on a previous pilot study, OCT centers from North America, Europe, and the Middle East combined resources to establish the basis for OCT-based detection of asymptomatic lesion in the optic nerve. For this purpose, the authors focused on the retinal nerve fiber layer (RNFL), consisting of the axons of retinal ganglion cells forming the optic nerve. During an ON attack, RNFL thickness transiently increases (due to inflammation-mediated edema of the optic nerve) but decreases thereafter by approximately 20%. To trace such a reduction and thus identify a prior episode of ON, reference ranges for the RNFL thickness are needed. However, this is challenging given interindividual variations, underlying ophthalmological conditions (eg, myopia), and different OCT devices or acquisition protocols. Nolan et al addressed the issue by measuring intereye differences in a standardized manner in a very large cohort, consisting of >1,500 MS patients, among them 477 patients with a history of previous acute unilateral ON, and appropriate healthy controls. This approach allowed the authors to verify a cutoff of 5μm intereye difference for the RNFL of an optic nerve with history of ON.Moreover, the authors identified further 240 patients with such an intereye difference >5μm but without reported history of ON. This was expected, because independent postmortem studies demonstrated lesions in the visual pathway of most MS patients, irrespective of a prior history of ON. Of note, whereas high-contrast visual acuity was not affected in these patients without reported history of ON, they showed a decrease in low-contrast letter acuity, known to be more sensitive to MS-related impairment. Clearly, the current study is one of the largest collaborative approaches in OCT research in MS, characterized by a sophisticated statistical analysis to adjust for a defined but nevertheless heterogeneous sample. Heterogeneity was predictable, given the mixed patient population, the restricted
Journal Title: Annals of Neurology
Year Published: 2019
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!