Photo from wikipedia
Correspondence Robert D. Safian, MD MSCAI, The Lucia Zurkowski Endowed Chair for the Center for Innovation and Research in Cardiovascular Diseases, Beaumont Hospital-Royal Oak, Royal Oak, MI 48073. Email: [email protected]… Click to show full abstract
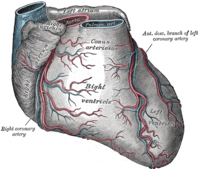
Correspondence Robert D. Safian, MD MSCAI, The Lucia Zurkowski Endowed Chair for the Center for Innovation and Research in Cardiovascular Diseases, Beaumont Hospital-Royal Oak, Royal Oak, MI 48073. Email: [email protected] Anomalous origin of the left (ALCA) or right (ARCA) coronary artery from the opposite sinus of Valsalva is a rare congenital condition that is usually identified incidentally by invasive coronary angiography (ICA) or by coronary computed tomography angiography (CT) during evaluation of patients with suspected myocardial ischemia. The risk of sudden cardiac death (SCD) and myocardial ischemia are higher in patients with an inter-arterial course (particularly of the left main coronary artery) between the pulmonary artery and aorta, when associated with “malignant” high-risk features including a slit-like orifice, acute angulation of the origin of the vessel from the aorta, and an intramural location in the aortic wall (Figure 1a); systolic compression is not the primary mechanism of ischemia or SCD. Most patients with SCD due to anomalous coronary arteries are <35 years old, so survival into the sixth and seventh decades may imply a lower risk of SCD. An inter-arterial course without high-risk features may not be associated with an adverse prognosis. “Benign” anomalies include anomalous origin from the opposite sinus of Valsalva in which high-risk features are absent; these include most patients with pre-pulmonic, sub-pulmonic (septal), and retro-aortic courses. Patients with ALCA/ ARCA may develop symptomatic coronary artery disease (CAD), so appropriate therapy may be impacted by CAD rather than by the anomaly per se. In this issue of Catheterization and Cardiovascular Interventions, Darki and colleagues detail their single center experience with percutaneous coronary intervention (PCI) and drug-eluting stents in 11 patients with ARCA from the left sinus, including acute coronary syndromes in 4 and abnormal functional testing in 6. ICA identified a high-risk inter-arterial course (n = 3) and sub-pulmonic course associated with significant CAD (n = 8). Intravascular imaging or invasive pressure measurements were not performed. Technical success was achieved in all patients, and there were 2 non-cardiac deaths and 2 target vessel failures after 8 years of follow-up. CT was performed in 10 patients at 1.5 years after PCI, to confirm the anomalous course and to assess stent integrity; none had stent fracture or deformation. The article confirms the feasibility of PCI in ARCA, but does not provide insight into prevention of SCD, nor does it clearly differentiate CAD from anomalous origin as a cause of ischemia. In our opinion, CT is the best technique to assess patients with coronary anomalies, and should be performed before revascularization in all patients with ALCA/ARCA to define the vessel course, the presence of high-risk morphological features (which may be missed by ICA), and the severity of CAD. For patients with “malignant” ALCA (left main) without CAD, surgical revascularization is considered a Class I recommendation; PCI has not been adequately studied. The preferred surgical approach may be unroofing and marsupialization of the intramural left main, recognizing that injury to the aortic valve can occur and may require aortic valve repair or Key Points
Journal Title: Catheterization and Cardiovascular Interventions
Year Published: 2020
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!