Photo from wikipedia
Over the course of the last decade transcatheter aortic valve replacement (TAVR) has been extensively performed and investigated for the treatment of patients with symptomatic severe aortic stenosis (AS) and… Click to show full abstract
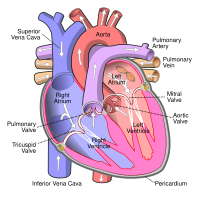
Over the course of the last decade transcatheter aortic valve replacement (TAVR) has been extensively performed and investigated for the treatment of patients with symptomatic severe aortic stenosis (AS) and is currently considered an alternative to surgical aortic valve replacement, even in younger, lower surgical risk patients. In addition, technological advancements and growing operators' experience, have brought TAVR to the treatment of bioprosthetic valve failure (BVF) and, more rarely, pure aortic regurgitation (AR). Although randomized clinical trials (RCTs) are lacking, the efficacy of the transcatheter aortic valve‐in‐valve (VIV) implantation in patients with BVF has emerged from large real‐world registries. In these studies, isolated severe regurgitation was the cause of BVF in almost one‐third of cases and was associated with a better survival rate than BVF due to restenosis. Nevertheless, increased risk for postprocedural elevated transvalvular pressure gradients (≥20mmHg), particularly in patients with small bioprostheses implanted (diameter ≤ 21mm), remains well‐ known, possibly hampering the hemodynamic improvements and long‐ term efficacy of VIV implantation. On the contrary, the available data on the use of TAVR for the treatment of severe native AR (NVAR) are scanter and, actually, NVAR remains an off‐label indication for TAVR. The lack of annular/leaflet calcification, the irregular and large orifice geometry, and the frequent association of ascending aorta pathology make the TAVR procedure much riskier compared to the AS setting, due to the higher risk of complications like device embolization, second valve implantation, and significant residual postprocedure paravalvular leak. Nonetheless, previous studies on this topic have shown TAVR feasibility and safety in patients deemed at high surgical risk or inoperable. In the largest study published on NVAR in high surgical risk patients, TAVR (n = 912) outcome was similar to surgically treated patients (n = 13,808) in terms of in‐hospital mortality both in unmatched and propensity‐matched cohorts. A favorable outcome of TAVR in pure NVAR was found also by others with the use of the oversized self‐expandable ACURATE neo device at the cost of a slightly higher need for permanent pacemaker implantation. Sawaya et al., comparing the outcome of TAVR for the treatment of isolated AR due to BVF or native valve (NV) disease, found that safety and efficacy were superior in the former group of patients. Furthermore, they highlighted the lower rate of moderate‐to‐severe residual AR after TAVR with new generation transcatheter heart valves (THV) compared to old generation devices. Similarly, the current study of Paraggio et al. explored the hemodynamic impact of new generation TAVR devices in patients with isolated AR, trying to find whether there is a significant interaction between AR in BVF versus NV disease patients. The Authors presented a retrospective evaluation of 28 patients who underwent successful TAVR with both invasive and noninvasive hemodynamic assessment by means of left ventricle (LV) catheterization before and after TAVR and echocardiography before, after (24–72 h) and at follow‐up (3–12 months). Regarding procedural data, both groups were treated with new‐ generation devices (comprising Evolut PRO, Evolut R, SAPIEN 3, and
Journal Title: Catheterization and Cardiovascular Interventions
Year Published: 2022
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!