Photo from wikipedia
We read with interest the recent paper written by Räsänen A. et al., entitled “Percutaneous Coronary Intervention with Drug‐Coated Balloon‐Only Strategy Combined with Single Antiplatelet Treatment in Patients at High… Click to show full abstract
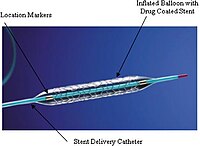
We read with interest the recent paper written by Räsänen A. et al., entitled “Percutaneous Coronary Intervention with Drug‐Coated Balloon‐Only Strategy Combined with Single Antiplatelet Treatment in Patients at High Bleeding Risk–Single Center Experience of a Novel Concept.” The concept of reducing the duration of antiplatelet treatment as well as the use of non‐stent therapy effectively treating some patient subsets, is an important treatment option that we do not have available in the United States. Räsänen et al. describes treatment of patients with de novo lesions with a drug‐coated balloon and a short duration of antiplatelet treatment. The authors report the fact that 40% of the patients were treated with a single antiplatelet agent for 1 month or less in their series. These were not low‐risk patients, with the average patient being 75 years of age. Interestingly, 15% of the patients had documented aspirin allergy and so did not receive even aspirin during the procedure. This article was timely for me in that I recently treated a 71‐year‐old female patient who presented with acute coronary syndrome and previous in‐stent restenosis with multiple layers of stents previously placed in her right coronary artery. She also had a history of anemia with a hematocrit of 25% and was receiving iron infusions because of a dietary absorption issue with iron. She previously had an evaluation for G.I. bleed with nothing found on upper or lower endoscopy. She presented during her procedure with a hematocrit of 35% after receiving several blood transfusions. Her angiogram again showed the in‐stent restenosis inside the proximal right coronary artery. Unfortunately, the vessel downstream was about 1.5mm in diameter but had excellent TIMI grade 3 flow. She clearly was not a candidate for surgical coronary revascularization of the right coronary artery with this small distal vessel. The authors point to the fact that this type of patient could be an excellent candidate for a drug‐coated balloon, which, unfortunately is not available in the states. As the authors delineate in their registry, drug‐coated balloon (DCB) only percutaneous coronary intervention (PCI) was shown to be noninferior to stenting in the BASKET–SMALL‐2 randomized controlled trial (RCT). In the past, we have been involved with several seminal trials using treatments other than stents for reduction in restenosis. We recently lost a friend and a colleague, Margolis et al., who published the first paper on use of an antiproliferative drug in patients to reduce restenosis. The SNAPIST trial was left by the wayside with the approval of the drug‐eluding stent, but it did show a significant reduction in restenosis in our small series. Unfortunately, there was a small incidence of short‐ term alopecia, something that would not be tolerated by myself or any of my patients. We reported a large series of patients treated with radiation to successfully reduce in‐stent restenosis. This article, authored by my co‐national PI of the START Trial, Dr. Jeffrey Popma, was the first large study describing this technique to combat restenosis. This technique is still effective but not available widely at centers. As this excellent retrospective registry describes, there are new treatment options that do not require us to place new drug‐eluding stents and appear to be not only effective but safe. There were no significant bleeding episodes in these patients, with a low incidence (2. 3%) of severe bleeding (BARC 3–5) at one‐year follow up. The one‐year MACE rate (4.7%) and the risk of cardiovascular death (2.9%) was surprisingly low in this high bleeding risk population. PCI mortality increases seven‐fold when bleeding occurs with the procedure. Despite the lack of DAPT after
Journal Title: Catheterization and Cardiovascular Interventions
Year Published: 2023
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!