Photo from wikipedia
AIMS The impact of hospital volume on clinical performance has been investigated by many researchers to date and thought that it is associated with quality of care and outcome for… Click to show full abstract
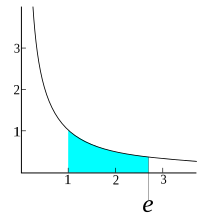
AIMS The impact of hospital volume on clinical performance has been investigated by many researchers to date and thought that it is associated with quality of care and outcome for patients with heart failure (HF). This study sought to determine whether annual admissions of HF per cardiologist are associated with process of care, mortality, and readmission. METHODS AND RESULTS Among the nationwide registry 'Japanese registry of all cardiac and vascular diseases - diagnostics procedure combination' data collected from 2012 to 2019, a total of 1 127 113 adult patients with HF and 1046 hospitals were included in the study. Primary outcome was in-hospital mortality, and secondary outcome was 30 day in-hospital mortality and readmission at 30 days and 6 months. Hospital and patient characteristics and process of care measures were also assessed. Mixed-effect logistic regression and Cox proportional-hazards model was used for multivariable analysis, and adjusted odds ratio and hazard ratio were evaluated. Process of care measures had inverse trends for annual admissions of HF per cardiologist (P < 0.01 for all measures: prescription rate of beta-blocker, angiotensin converting enzyme inhibitor or angiotensin II receptor blocker, mineralocorticoid receptor antagonist, and anticoagulant for atrial fibrillation). Adjusted odds ratio for in-hospital mortality was 1.04 (95% confidence interval (CI): 1.04-1.08, P = 0.04) and 30 day in-hospital mortality was 1.05 (95% CI: 1.01-1.09, P = 0.01) for interval of 50 annual admissions of HF per cardiologist. Adjusted hazard ratio for 30 day readmission was 1.05 (95% CI: 1.02-1.08, P < 0.01) and 6 month readmission was 1.07 (95% CI: 1.03-1.11, P < 0.01). Plots of the adjusted odds indicated 300 as the threshold of annual admissions of HF per cardiologist for substantial increase of in-hospital mortality risk. CONCLUSIONS Our findings demonstrated that annual admissions of HF per cardiologist are associated with worse process of care, mortality, and readmission with the threshold for mortality risk increased, emphasizing the optimal proportion of patients admitted with HF to cardiologist for better clinical performance.
Journal Title: ESC heart failure
Year Published: 2023
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!