Photo from wikipedia
For clinicians caring for patients with heart failure (HF), acute or chronic kidney disease (CKD), and/or diabetes mellitus, dyskalaemia and optimization of diuretics and renin– angiotensin–aldosterone system inhibitors (RAASi) are… Click to show full abstract
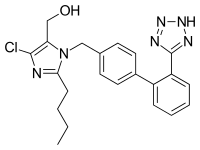
For clinicians caring for patients with heart failure (HF), acute or chronic kidney disease (CKD), and/or diabetes mellitus, dyskalaemia and optimization of diuretics and renin– angiotensin–aldosterone system inhibitors (RAASi) are everyday concerns. Although we understand cellular and renal potassium regulation, surprisingly little is known about the causal relationships between these syndromes, drug effects, and outcomes. In this issue of the Journal, Beusekamp et al.1 studied potassium, use of RAASi drugs, and outcomes in patients with HF and reduced ejection fraction (HFrEF) from the well characterized longitudinal BIOSTAT-CHF cohort. At baseline, hypokalaemia (K< 3.5 mEq/L) was present in 6.9% and hyperkalaemia (K> 5.0 mEq/L) in 8.0%. In unadjusted and adjusted Cox models, neither hypoor hyperkalaemia, nor increases or decreases in potassium at 9 months, were significantly associated with the composite outcome of all-cause death or HF hospitalization up to 2 years. However, in univariable and several multivariable logistic regression models, higher baseline potassium was associated with lower odds of angiotensin-converting enzyme inhibitor (ACEi)/angiotensin receptor blocker (ARB) uptitration. So is hyperkalaemia a risk marker or a risk factor for poor outcomes in HF? Does dyskalemia cause poor outcomes? Several studies indicate that the relationship between potassium and outcomes exhibits a U-shaped relationship in HF and/or CKD.2,3 However, the extent of multivariable adjustment in these studies has been variable. In the present analysis, hypoor hyperkalaemia were not significantly associated with outcomes. However, the sample size of 1666 was
Journal Title: European Journal of Heart Failure
Year Published: 2018
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!