Photo from wikipedia
In the last decade, the left atrium has been recognized as an independent factor involved in the pathophysiological process of multiple cardiovascular diseases.1,2 Left atrial (LA) dilatation and impaired LA… Click to show full abstract
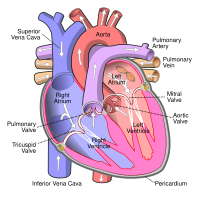
In the last decade, the left atrium has been recognized as an independent factor involved in the pathophysiological process of multiple cardiovascular diseases.1,2 Left atrial (LA) dilatation and impaired LA function are associated with an increased risk of hospitalization for heart failure (HF) and mortality in the general population as well as in patients with HF with preserved (HFpEF) and reduced ejection fraction (HFrEF).3–5 Although the left atrium had been commonly considered a buffer chamber between the pulmonary circulation and the left ventricle, increasing evidence suggests that LA ‘remodelling’ does not represent an innocent bystander, but rather plays an active role in the pathophysiology and development of HF.6 Indeed, the term ‘atrial failure’ has recently been proposed as a clinical entity, characterized by any anatomical, mechanical, or electrical dysfunction causing impaired heart performance and symptoms.7 Many clinical studies have shown the beneficial effect of pharmacological and device therapy on changes in left ventricular (LV) structure and function and demonstrated that reverse LV remodelling is associated with lower rates of subsequent cardiovascular events.8 Yet, similar evidence assessing the favourable effects of targeted medical therapy on LA structure and function and its prognostic implications is lacking.9 Therapeutic interventions may attenuate LA enlargement and dysfunction in patients both from the general population and those with prevalent HF. From this perspective, assessment of LA changes may represent a useful marker that captures the treatment effect on overall LA health (e.g. LA cardiomyocyte function, degree of LA fibrosis). Moreover,
Journal Title: European Journal of Heart Failure
Year Published: 2022
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!