Photo from wikipedia
In this issue you find a paper by Hazime et al., entitled, “Treating low back pain with combined cerebral and peripheral electrical stimulation: A randomized, double-blind, factorial clinical trial” (Hazime… Click to show full abstract
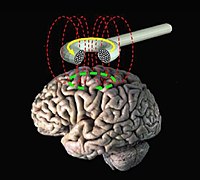
In this issue you find a paper by Hazime et al., entitled, “Treating low back pain with combined cerebral and peripheral electrical stimulation: A randomized, double-blind, factorial clinical trial” (Hazime et al., 2017). The authors present an efficacy trial of transcranial direct current stimulation (tDCS) combined with peripheral electrical stimulation (PES) over four treatment weeks in a sample of 92 patients with chronic low back pain. Although tDCS and PES are both non-invasive forms of electrical stimulation, tDCS acts at the cerebral level whereas PES acts peripherally via nerve sites. Compared to participants who underwent tDCS or PES alone or a sham control, the combined tDCS-PES group demonstrated maintenance of analgesic effects and perceived global improvement in their condition at 3 months post-treatment as well as a higher proportion of responders to treatment at different cutoff points. This is one of the largest studies of noninvasive neuromodulation in pain, and it ranks among those with the largest number of maintenance sessions. This manuscript reflects a promising new treatment approach for low back pain, as well as persistent pain more generally. At present, effective treatments for persistent pain are limited, despite common application of pharmacological (largely opioid) as well as exercise and psychological treatments. In isolation, most common treatments produce only small effects sizes. The development of non-invasive brain stimulation techniques for the relief of pain, which provide a more direct method to target central nervous system changes in chronic pain, was originally welcomed with hope that clinical benefits greater than those of commonly used therapies would be elicited. Over time, enthusiasm has been challenged by the publication of meta-analyses suggesting at best, modest effects on pain. However, addressing the success of brain stimulation for pain relief in systematic reviews has been problematic given the literature consists predominantly of proofof-concept studies with heterogeneous methods (e.g. target sites, stimulation parameters and treatment durations), pain populations and stimulation techniques/protocols. Also, head-to-head studies have rarely been performed. In addition, an important question is whether the modest benefits reported when non-invasive brain stimulation is used as a monotherapy, are enhanced when non-invasive brain stimulation is used as an adjunct to traditional therapy (e.g. peripheral electrical stimulation, exercise). In fact, while tDCS failed to provide significant analgesic relief when used alone, it has the potential to create additive effects on pain system function when applied in combination with an adjunctive technique, as reported by Hazime et al.,. tDCS is thought to work through long-term potentiation-like (LTP; the strengthening of synapses between nerve cells) effects on stimulated neurons, potentially increasing the brain’s responsiveness to a second therapy that activates the same neural circuits. The data of Hazime et al. suggest tDCS of the primary motor cortex combined with peripheral electrical stimulation of the back may induce additive effects that prolong the analgesic effect of either treatment applied alone. Although further research is needed to confirm this effect in chronic LBP, there is an emerging evidence base to support combined noninvasive brain stimulation and traditional therapies in the field of pain and more broadly, such as in Major Depressive Disorder. This includes non-invasive brain stimulation combined with a range of psychological interventions including mindfulness therapy and Cognitive Behavioural Therapy (CBT) as well as exercise and physical therapy. A critical consideration is that non-invasive brain stimulation must be applied to an appropriate target region that allows synergistic neural effects. For instance, a recent study showed no
Journal Title: European Journal of Pain
Year Published: 2017
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!