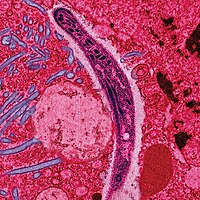
Photo from wikipedia
cell lymphoma (DLBCL), salvage chemotherapy prior to autologous stem cell transplant (HSCT) remains the standard approach at relapse. However, there is no consensus salvage regimen and practice varies considerably. Refractory… Click to show full abstract
cell lymphoma (DLBCL), salvage chemotherapy prior to autologous stem cell transplant (HSCT) remains the standard approach at relapse. However, there is no consensus salvage regimen and practice varies considerably. Refractory DLBCL or short remission duration cases have particularly poor outcomes (Gisselbrecht, 2010). R-IVAC is an infusional protocol incorporating etoposide (60mg/m Day 1-5), ifosfamide (1.5g/m Day 1-5), cytarabine (2g/m BD Day 1-2) in addition to Rituximab (375mg/m). Methods: We retrospectively analysed 27 patients treated at two teaching hospitals to determine the safety and efficacy of R-IVAC for relapsed DLBCL. Disease response was assessed by PET (Lugano 2014 criteria). Results: Patient characteristics are summarised in Table 1. 13 patients (48%) were refractory to their previous therapy and 9 patients (33%) had relapsed in <12 months. 70% of patients received 2 cycles of treatment (range 1-3) and 92.5% received rituximab with IVAC. In 26 evaluable patients, the overall response rate (ORR) was 54% (42% complete response, 12% partial response). In patients with disease relapsing after >12 months, the ORR was 100%, versus 43% in relapses <12months or refractory disease. 21 patients were referred for HSCT, and 10 (37%) patients proceeded (9 autograft, 1 allograft). Stem cell mobilisation succeeded in 90% of patients. 2 patients declined HSCT, 8 did not proceed due to inadequate disease control. With a median duration of follow-up in surviving patients of 30 months, 2-year progression-free survival (PFS) of the whole cohort was 25% and 2-year overall survival (OS) was 32%. Patients who responded achieved 2-year PFS of 53% and OS of 62%. In HSCT recipients, 2-year PFS and OS were 44% and 66%. Hematologic toxicity was considerable with grade 3/4 neutropenia and thrombocytopenia in 92.5% and 100% patients respectively. 25 patients experienced febrile neutropenia, but only 1 patient died of treatment-related toxicity. The mean hospital length of stay per cycle was 15.6 days. 18 patients required an unplanned admission. Conclusion: R-IVAC demonstrated significant therapeutic efficacy and manageable toxicity in a cohort overwhelmingly composed of refractory or early relapse DLBCL, perhaps suggesting therapy intensification to be effective in refractory disease. Judicious patient selection is required given the rate of toxicity.