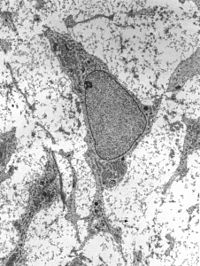
Photo from wikipedia
Introduction: Ibrutinib with rituximab (IR) combination induces durable responses in relapsed MCL. This is a single institution phase II trial of IR with short course (4 cycles) of R-HCVAD/R-MTX consolidation… Click to show full abstract
Introduction: Ibrutinib with rituximab (IR) combination induces durable responses in relapsed MCL. This is a single institution phase II trial of IR with short course (4 cycles) of R-HCVAD/R-MTX consolidation as frontline therapy in MCL. Methods: Previously untreated young (≤65 years) MCL pts (n=50) were included. The study was registered with a ClinicalTrials.gov identifier number NCT02427620. Pts received IR induction (part-A), until they achieved complete remission (CR) up to a maximum of 12 cycles, followed by only 4 cycles of R-HCVAD/R-MTX (part-B). None of the patients received stem cell transplant or maintenance. The primary objective was to assess response rates after part-A. Among evaluable samples, minimal residual disease (MRD) by flow cytometry at best response, clonal evolution using circulating tumor DNA (ctDNA) at various time points, baseline somatic mutations and baseline gene expression profile (GEP) was performed. Results: Overall, the median follow up was 36 months (10-42). Forty nine percent had high Ki-67 (≥30%), 72% had low risk MIPI score, one pt had TP53 mutation and 2 pts had aggressive MCL (one blastoid and one pleomorphic). Median number of cycles on IR was 6 (2-12). Overall response (ORR) on part-A of therapy was 100% (90% CR and 10% PR) and at the time of last follow up after completion of part A and part B, ORR was 100% (All CR). MRD negative CR rate assessed by bone marrow flow cytometry performed at best response at any phase of treatment was 91%. Overall, the median PFS and OS were not reached (3 year 89% and 100% respectively). Four pts had progressed after 17, 24, 34, 35 months of treatment (3 pts had Ki-67% ≥ 30% and one was blastoid MCL). None of the pts died. Grade 3-4 toxicities on part A were 4% myelosuppression and 8% each with fatigue, myalgia and rashes. GEP was done in 18 pts (2 PR, 16 CR on part A). Pts in PR had higher expression of HES1while those in CR had significantly higher expression of CTLA4 and ITK genes compared to those in PR. Targeted DNA sequencing was done in 18 pts at baseline, one pt with PR had NSD2, KMT2C and another pt had TP53 mutations and had CR. Conclusions: IR followed by short course R-HCVAD/R-MTX as frontline treatment induced durable and profound remissions in young MCL pts. This strategy demonstrated excellent efficacy and safety and minimized the exposure to chemotherapy.