Photo from wikipedia
I n this issue of JBMR, Jan de Beur and colleagues (1) report the primary analysis and findings up to closure of their prospective, open-label, single-arm, phase 2 study (NCT02304367)… Click to show full abstract
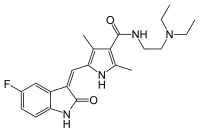
I n this issue of JBMR, Jan de Beur and colleagues (1) report the primary analysis and findings up to closure of their prospective, open-label, single-arm, phase 2 study (NCT02304367) to evaluate the safety and efficacy of burosumab-twza for treating adults with a debilitating disorder, tumor-induced osteomalacia (TIO). Burosumab is the fully human monoclonal antibody against the phosphatonin fibroblast growth factor-23 (FGF23). Their clinical trial was sponsored and funded by Ultragenyx Pharmaceutical, Inc., in partnership with Kyowa Kirin International, plc (UX023T-CL201). Beginning in 2015 at six sites in the United States, 20 individuals were screened and 17 enrolled, leading to evaluation of 14 men and women with elevated serum FGF23 levels and said to have TIO for which surgical resection was not possible or curative. Also, one adult, to be reported elsewhere, was studied with what has been called epidermal nevus syndrome with hypophosphatemic rickets, but is now referred to as cutaneous skeletal hypophosphatemia syndrome (CSHS). Our observations from the first such patient treated with burosumab, a boy, predict their findings will be positive. In both TIO and CSHS, elevation of circulating FGF23 is acquired and causes renal wasting of inorganic phosphate (Pi) and consequently hypophosphatemic rickets or osteomalacia. For decades, both entities have been managed medically using a relatively inexpensive, but not always adhered to, cumbersome regimen of one or two oral doses daily of a bioactive form of vitamin D3, ie, calcitriol [1,25(OH)2D3] or alfacalcidol [1α(OH)D3], together with four or five oral doses each day of a Pi salt, aiming to compensate for the hyperphosphaturia and hypophosphatemia by transiently increasing circulating “phosphorus” (P) levels. Evenwith skilled management, this somewhat simplistic approach to the pathogenesis of TIO and CSHS risks nephrocalcinosis with impaired renal function, and secondary or tertiary hyperparathyroidism. In the study discussed herein, to better target the pathogenesis of the renal Pi wasting in TIO while also facilitating treatment compliance, the participants received burosumab subcutaneously once every 4 weeks, with the maximum single dose set at 2 mg/kg body weight. Dose adjustments, aimed to achieve the pharmacodynamic endpoints, were based on fasting serum P levels assessed especially often during the initial titration phase of 16 weeks. The protocol, amended six times from 2014 to 2019, and the results are further detailed in the linked Supplemental Appendix S1 of 120 pages. The overall findings reflect 144 weeks (2 years, 9 months) of therapy, and by study completion a mean single dose of 0.7 mg/kg. The co-primary endpoints were: (i) the proportion of patients with an average fasting serum P level >0.81 mmol/L (ie, >2.5 mg/dL) at the midpoint of the dose interval between baseline and week 24 (adult normal range 0.81–1.29 mmol/L; ie, 2.5–4.0 mg/dL), and (ii) change in histomorphometric parameters of osteomalacia assessed by iliac crest biopsy at baseline and week 48. Ten subjects with TIO completed the study. Mean serum P increased early on, with 7 of the 14 patients (50%) achieving the targeted P level. Then, the level was sustained, testing at the endpoint of the dose interval. The mean value increased for the ratio of the renal tubular maximum reabsorption rate of Pi to glomerular filtration rate (TmP/GFR) but never entered the normal range. Mean serum parathormone levels were elevated at baseline and then decreased but did not correct, perhaps reflecting persisting parathyroid gland hyperplasia. Iliac crest histomorphometry of 11 participants showed most key parameters of osteomalacia were not statistically improved or corrected. Bone turnover markers in serum were normal and essentially unchanged. Two subjects did not meet the histomorphometric criteria for osteomalacia at baseline, and another two were excluded after week 48 when a protocol amendment requiring specifically PHEX gene analysis revealed they had X-linked hypophosphatemia (XLH). Four of the 14 patients were considered to have TIO, yet a neoplasm had not been located, said to be common for TIO in relatively old publications, even after GaDOTATATE PET/CT was added to the protocol. Normal stature and late onset of symptoms were considered evidence against a congenital disorder. With burosumab treatment, improvements were reported in clinically important parameters. Tests of functional mobility and the SF-36v2 health survey and brief pain and fatigue inventories showed treatment benefits. Whole-body bone scintigraphy indicated that by study end, many, but still a minority, of fractures and pseudofractures were healed or partially healed. The safety profile for burosumab was provided in detail and reassuring, with adverse events of interest beingmild tomoderate. The serious adverse events were considered unrelated to burosumab treatment. Renal sonography showed no increase in nephrocalcinosis or development of kidney stones. No neutralizing anti-burosumab antibodies were detected. I do wonder if any of the four study subjects never with an identified tumor (none was tested for a PHEX mutation) had a heritable hypophosphatemia, particularly the 30-UTR c.*231A > G mutation in PHEX we reported in 2015 in JBMR to cause a mild variant of XLH, thus far not uncommon yet uniquely in the United States and sometimes presenting in adult life. Hence, in such individuals, positive mutation analysis, perhaps on exome sequencing or from a panel of genes associated
Journal Title: Journal of Bone and Mineral Research
Year Published: 2021
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!