Photo from wikipedia
The paradigm “time is brain” has been challenged by the advances in diagnostic neuroimaging to such an extent that, for acute ischemic stroke, the decision to perform intravenous thrombolysis or… Click to show full abstract
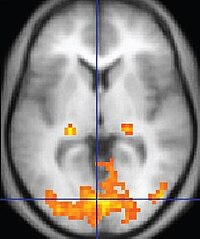
The paradigm “time is brain” has been challenged by the advances in diagnostic neuroimaging to such an extent that, for acute ischemic stroke, the decision to perform intravenous thrombolysis or mechanical thrombectomy nowadays relies more on computed tomography (CT) or magnetic resonance imaging (MRI) findings, rather than on the time elapsed from symptoms onset. A recent systematic review and meta-analysis reported improved outcomes for patients treated more than 4.5 h after onset, or with wake-up stroke, being imaged and selected for thrombolysis based on perfusion imaging. Actually, endovascular thrombectomy for large vessel occlusion may be offered up to 24 h after onset of ischemic stroke symptoms. The availability of such advanced imaging techniques on a large scale is crucial, as much as it is the local expertise and resources to perform functional studies like perfusion. The paper entitled “Comparison of Magnetic Resonance Imaging vs. Computed Tomography-based thrombolysis treatment in patients with acute ischemic stroke” which has been recently published in the Journal of Clinical Ultrasound, offers an interesting insight in this field. Although the authors did not go far into details for what concerns the imaging techniques they used, they observed an advantage in terms of reduced mortality and bleeding events when patient selection for thrombolytic therapy was based on MRI; parallel, they did not observed any significant differences in midterm functional outcomes. These findings support other literature data that show the superiority of MRI compared to CT in ischemic core determination, which may improve patient management. Despite a slight increase in the time delay between diagnosis and treatment, MRI is still considered the gold standard for the most accurate estimation of infarct volume, which is the crucial aspect in particular when the early time window has elapsed. However, this information should be taken with caution for several reasons. First, most of the clinical trials performed in recent years did not necessarily require advanced neuroimaging for the indication to revascularization therapies that provided positive functional clinical outcomes to patients. In a systematic review and meta-analysis, Tsivgoulis et al. found that among 10 randomized controlled trials assessed, only five relied on perfusion imaging for patient selection. This proves not only that conventional CT imaging presents an acceptable accuracy and good prognostic value, but also that it is widely available and its interpretation is relatively simple. Hendrix et al. showed that patients selected for mechanical thrombectomy in the extended time window solely based on noncontrast-CT and CT-angiography, achieved favorable functional outcomes at 3 months, comparable to those in patients in the early time window. In addition, Nogueria et al. in a post hoc analysis of a large prospective registry found that extended window patients might be safely treated in the absence of CT perfusion (CTP) or MRI data. However, evidence is growing from randomized controlled trials that CTP can be considered a reliable tool as well as MRI, for patients selection to revascularization therapy, both in the early time window as well as in the late, from 6 to 24 h. Indeed, none of these trials had as endpoint the comparison between CTP and MRI and the results of the subgroup analysis did not show significant differences, although with limited statistical power. Campbell et al in the HERMES collaboration pooled patient-level data from seven randomized trials and they found that diffusion MRI was associated with better outcomes at any estimated ischemic core volume; however, the difference was minimal and prognostic accuracy between diffusion MRI and CTP was comparable. Nevertheless, diffusionand perfusion-weighted MRI is still considered the gold standard for ischemic core and penumbra determination and several authors still claim the superiority of diffusionweighted MRI compared to CTP, especially to identify those patients who would not benefit from revascularization therapy due to the risk of hemorrage. Despite this, recent advantages in CTP technology, standardization of protocols and results interpretation are leading to an increased confidence towards CTP, also thanks to the development of automated analysis software, which aim to reduce visual image Received: 17 December 2021 Revised: 19 December 2021 Accepted: 20 December 2021
Journal Title: Journal of Clinical Ultrasound
Year Published: 2022
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!