Photo from wikipedia
The study of fetal heart is a routine part of the obstetrics ultrasonography. According to all the major guidelines the standard evaluation is focused on the visualization of the four… Click to show full abstract
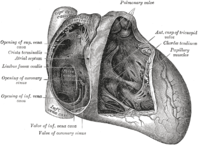
The study of fetal heart is a routine part of the obstetrics ultrasonography. According to all the major guidelines the standard evaluation is focused on the visualization of the four chamber view, outflow tracts and more recently by the three vessels trachea view. The visualization of the systemic venous return is not performed routinely in particular the visualization of the inferior vena cava (IVC). Although inferior vena cava anomalies may be suspected by the visualization of the abdominal plane or 4 chamber view their diagnosis require a parasagittal view of the fetal trunk (Figure 1). Among caval anomalies Interrupted inferior vena cava (IIVC) (also known as azygos continuation of the inferior vena cava) is the most frequent vascular anomaly, with prevalence of about 0.2%–3%. IIVC is the result of fusion failure of one if the different portion of the embryological IVC. The embriogenesis of IVC is a complex process involving the formation of several anastomoses between three paired embryonic veins. Interruption of IVC with azygos continuation represents the most common abnormality involving these veins. The IVC is composed of four portions: hepatic, prerenal, renal and postrenal. These portions originate from the formation, fusion and regression of the cardinal veins. The azygos system is derived from the supra cardinal veins. Failure to fuse of the prerenal segment with the caudal portion of the hepatic segment results in interrupted IIVC and venous flow beyond the interruption proceed through the azygos system draining into the right atrium via the superior vena cava. The incidence of this anomaly is higher, in fetuses with a wide variety of anomalies involving visceral organs and the heart. Visceral heterotaxy, atrio ventriculat septal defects, anomalously connecting pulmonary veins, double outflow right ventricule, pulmonary stenosis left atrial isomerism (polysplenia syndrome) and right atrial isomerism (asplenia syndrome) have been most frequently associated with this vascular anomaly. In this issue Babao glu et al. reported how IIVC may be present also in fetuses without any cardiac anomalies. Indeed Authors found on 7250 fetal echocardiographic examination 36 cases of IIVC (0.5%). Of these 36 cases 22 were associated with a congenital heart disease while the remaining 14 were isolated (38.8%). However in 6 cases of the latter group despite a normal heart visceral abonormalities were present including anomalies of the spleen (right position and polysplenia) and right position of the stomach. Anomalies of the spleen were diagnosed postnatally in most of the cases. These findings in agreement with pediatric series and at autopsy. The identification of apparently isolated IIVC is of clinical interest since they may express in adult life an higher possibility of developing arrhythmia with an increased the likelihood of development of sick sinus syndrome in future, increased risk for deep venous thrombosis. Further the association of coronary anomalies has been reported. These findings suggest that incorporating bicaval view in the study of the fetal heart may be is useful in identifying IVC defects and related anomalies. The use of three-dimensional volume analysis and artificial intelligence algorithm may greatly facilitate this process. Under this condition is first necessary a careful search for other intracardiac and extracardiac structural anomalies. Indeed associated anomalies may be underdiagnosed during prenatal life due to difficulties in prenatal identification of the spleen, visceral position and atrial appendages. As a consequence the apparent normal anatomic findings during prenatal life should be confirmed by postnatal evaluation by F IGURE 1 Sagitall view of the fetal thorax showing the inlet of inferior (IVC) and superior vena cava (SVC) in the left atrium Received: 19 March 2022 Revised: 21 March 2022 Accepted: 23 March 2022
Journal Title: Journal of Clinical Ultrasound
Year Published: 2022
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!