Photo from wikipedia
Editorial for “Convolutional neural network for accelerating the computation of the extended Tofts model in dynamic contrastenhanced magnetic resonance imaging” Dynamic contrast-enhanced (DCE) magnetic resonance imaging (MRI) can be a… Click to show full abstract
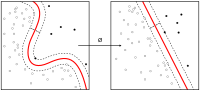
Editorial for “Convolutional neural network for accelerating the computation of the extended Tofts model in dynamic contrastenhanced magnetic resonance imaging” Dynamic contrast-enhanced (DCE) magnetic resonance imaging (MRI) can be a valuable tool for quantifying blood–brain barrier leakage and can also be used to derive quantitative imaging biomarkers in the field of oncology. The amount of data obtained in DCE-MRI is immense and needs to be further processed to obtain comprehensible and actionable information. Commonly, this processing step is performed by estimating the pharmacokinetic (PK) parameters related to changes in contrast agent in the tissues of interest over time. Several PK models exist, from simple to complex, and best model selection is tissue type dependent. One of the most commonly used models for estimation of the PK parameters is the Tofts and the extended Tofts (eTofts) model. In these models, the DCE-MRI time-series data are fitted on a voxel-wise basis using iterative nonlinear least squares (NLLS) fitting. The accuracy with which the PK parameters can be obtained is dependent on the contrast to noise ratio, the time resolution, and the accuracy of the arterial/venous input function (IF). Inherent to the voxel-wise data processing, the calculation time is directly proportional to the number of voxels of interest, and imaging noise is not mitigated within the PK parameter estimation. In this issue of JMRI, Fang et al. report on a deep learning-based approach to obtain the PK parameters from DCE-MRI using the eTofts model, aiming for substantially reducing the computation time without compromising on the accuracy. The used convolutional neural network consists of two parallel pathways, one focusing on the long-term and one on the short-term temporal information, in a different manner than the recently published approach by Zou et al. Results nicely illustrate that the long-term pathway benefits the accuracy of the PK parameter estimations. The paper goes further then just presenting the performance of a novel convolutional neural network (CNN) on PK parameter estimation. It also describes different strategies for training of the network, including real-world and artificially generated training data. They furthermore show that the network trained on glioma patients also performs well in external data of patients with brain metastasis and lymphoma patients, implying some generalizability. And finally, they also show that the CNN-based solution is more robust against added Gaussian noise compared to classical NLLS. The main aim of the paper, reducing computation time without compromising the accuracy has clearly been achieved. On a 32 CPU system NLLS takes 39.1 s to fit 10.000 voxels, while the CNN only takes 2.6 s. On a GPU this is further reduced to 0.33 s. With normalized root-mean-square errors between 1% and 4%, the accuracy is not compromised for the PK parameters. Reduction of the computation time to below 1 s is impressive, but it is questionable if it makes an actual difference for patients. Only in an acute setting, for example, assessing damage in a stroke patient, this could have an impact. For oncology patients, the time reduction might be less important. To really make impact, the speed-up should actually be a starting point for further improving the accuracy of DCE-MRI modeling. Benou et al., for example, showed that deep neural networks can be used to denoise DCE-MRI. With CNN’s, it is also possible to perform the calculations in a regional fashion, instead of voxel-by-voxel, enabling noise-mitigation within the PK parameter estimation steps. CNN’s can also be used to improve the robustness and accuracy on determined arterial/venous input function. Finally, with high-speed calculations it is also possible to compare different PK models and select the best model per tissue type. The main challenge for using artificial intelligence to further improving the pharmacokinetic modeling of DCE-MRI is that proper ground truth training data are generally missing. Like in the current paper, the best you can do is compare to NLLS fitted data, but what when you want to do better? The same holds for comparing automated arterial/venous input functions with observer dependent manually segmented regions. Systematically acquired test–retest data, as suggested in by the quantitative imaging biomarker alliance, might be one of the essential steps.
Journal Title: Journal of Magnetic Resonance Imaging
Year Published: 2021
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!