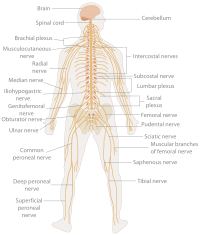
Photo from wikipedia
As its name would suggest, Neuroscience research has the neuron as its central focus. But much like we have come to recognize that, with genetics comes epigenetics, our views of… Click to show full abstract
As its name would suggest, Neuroscience research has the neuron as its central focus. But much like we have come to recognize that, with genetics comes epigenetics, our views of neurons acting in isolation have also evolved. We now recognize that there is a much more complex pallet of interacting cell types and neurons do not function in isolation. The classical neuroscience textbook diagrams of a presynaptic and postsynaptic terminal speaking to each other are now colored with additional players who can listen to the neuronal conversation and even partake in it. We now often speak of the “tri-partite” synapse and have come to recognize that glial cells such as astrocytes and microglia are intimately involved in this conversation. This In Focus Issue on Neuro-immune interactions in pathological states is aimed at further exploring the dynamic interactions of neurons and non-neuronal elements in the diseased nervous system. The reviews and primary research presented in this issue are intended to act as a primer on some of the fundamental mechanisms of glial and immune driven pathology from spinal cord injury to neuropathic pain. A key feature of this collection is that each paper examines pathological neuro–immune interactions in a different context and presents emerging strategies to counteract some of the potentially harmful outcomes that emerge from this cross-talk. A primary example of the nervous systems’ susceptibility to the influences of glial and peripheral immune cells is in cases of autoimmune pathology. In these disorders, dysregulation of the immune system leads to the targeting of specific antigens in the central nervous system or peripheral nervous system (CNS/PNS) with deleterious consequences. The prototypical autoimmune disease is multiple sclerosis (MS). The review by Yong, Chartier, and Quandt, Modulating inflammation and neuroprotection in MS stands as an excellent primer on the pathological mechanism of the disease, exploring the specific mechanisms of myelin and neuronal/axonal injury in MS and its animal model, experimental autoimmune encephalomyelitis. Their paper highlights the fact that while immune modulatory therapies may be the gold standard for treatment, neuroprotective approaches must also be considered given the links between disease progression and neurodegeneration. They place particular emphasis reviewing the data on some of the outcomes of immune-mediated attack of CNS antigens, namely oxidative stress and mitochondrial dysfunction as drivers of this pathology. They go on to discuss the evidence demonstrating the efficacy of approaches aimed at reducing oxidative stress and normalizing mitochondrial function in the disease. Understanding how the immune system becomes dysregulated in disease like MS has been a major focus of autoimmune research. The discovery of a special class of immunosuppressive T-cells, the T-regulatory cells (Treg) is the focus of the review provided by Duffy, Keating, Perera, and Moalem-Taylor, The role of regulatory T cells in nervous system pathologies. Duffy and colleagues dissect and discuss the complex role of the Tregs in autoimmunity (MS) but also discuss their influence on a variety of other nonautoimmune conditions. They highlight data demonstrating the modulatory influence of Tregs in animal models of neuropathic pain and their ability to regulate pathology after traumatic CNS injury or in neurodegenerative disorders like Amyotrophic Lateral Sclerosis, Alzheimers’, and Parkinson’s disease. This work illustrates how dysfunction in a specific class of peripheral immune cell, that normally quells inflammatory responses, can have a major impact on processes throughout the nervous system, from the processing of sensory signals in the spinal dorsal horn to the regulation of neuronal survival in the brain or motor neuron pools of the spinal cord. The review by Kopper and Gensel on the other hand, addresses neuro–immune interactions in the context of determining what drives the deleterious proinflammatory response in the CNS. Their review, Myelin as an inflammatory mediator: Myelin interactions with complement, macrophages, and microglia in spinal cord injury focuses on the chronic inflammatory setting of the injured spinal cord where myelin lipid debris is abundant. In this setting, damaged myelin acts as potent stimulator of macrophages, complement activation, and inflammation. The review covers the specific pathways that lead myelin to drive macrophages into a pathological/proinflammatory activation state or alternatively, a state that is reparative and anti-inflammatory. Although not inherently proinflammatory, myelin is capable of triggering proinflammatory and detrimental outcomes through the activation of phagocytes. The authors demonstrate that a more thorough understanding of the signaling pathways that lead to this detrimental activation state may identify novel therapeutic targets to prevent the excessive spread of damage in the injured spinal cord or even enhance endogenous growth and repair mechanisms. Salamone, Bernick, and Hines shift our focus to how neuroinflammatory processes impact on brain metabolism and the role of the mitochondria in this process. In their review, TSPO regulation in reactive gliotic diseases, the authors address the metabolic demands in the brain and how inflammatory processes can impact and disrupt proper brain
Journal Title: Journal of Neuroscience Research
Year Published: 2018
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!