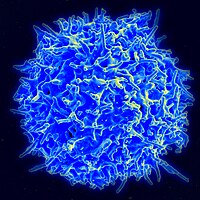
Photo from wikipedia
I have read the article entitled “Is Ethmoidal Air Cell Count Relevant in Chronic Rhinosinusitis?” with great interest. Main idea of the article is based on the knowledge that increased… Click to show full abstract
I have read the article entitled “Is Ethmoidal Air Cell Count Relevant in Chronic Rhinosinusitis?” with great interest. Main idea of the article is based on the knowledge that increased septation of the ethmoid could restrict ethmoidal drainage function and increased numbers of ethmoid cells (EC) could narrow ventilation pathways of the paranasal sinus as mentioned in the article. The authors found increased numbers of ethmoidal air cells in chronic rhinosinusitis (CRS) groups compared to healthy and odontogenic CRS control groups. Cell count could contribute to the pathogenesis of CRS. Even though the study brings a new insight into the understanding of pathogenesis of CRS, the study design includes several scientific flaws. Even though the authors have mentioned multifactorial pathogenesis incorporating extrinsic and intrinsic factors as an underlying cause of CRS in discussion section, they did not include these possible factors to their study to be analyzed. Main factors contributing to CRS pathogenesis are allergy, anatomic variations, frequent upper respiratory system infections, significant septal deviation, and smoking. These could have been added easily, and multifactorial regression analysis could have shown the leading cause. A study ignoring these factors and based on ethmoidal cell count solely would lead to defective speculations. Presence of allergy in an individual with a cell count even less than that of someone else without allergy could lead to CRS. Likewise, septal deviation and large choncha bullosa obstructing osteomeatal complex might contribute to CRS pathogenesis. Other anatomic variations narrowing nasofrontal duct might lead to CRS irrespective of EC count. Another striking finding is that multiplication of total sagittal and axial EC count (median values) in CRS groups significantly increased the difference between in CRS groups and other groups (36 and 38 vs. 54 and 59) whereas there was not big difference between in CRS groups and other groups when total sagittal (13 and 14 vs. 14 and 16) or axial cell count (12 and 11 vs. 14 and 15) was considered. Furthermore, as noted in table I, total sagittal and axial EC counts are so close to each other in each group. It is interesting to note little differences with significant comparisons even in case of small patient and subject populations. Final points are timing of taking CT and issue of presence or absence of active infection. Presence of active infection (seems opacification on CT) in a patient with increased number of EC might cause misclassification that patient into CRS group without polyp. However, antimicrobial treatment might resolve opacification on the paranasal sinus. Therefore, the authors should declare that the patients were infection-free at the time of taking computed tomography. This condition is not the case for CRS group with nasal polyp. Any of these thoughts does not serve to deny role of increased number of EC in CRS pathogenesis. In contrary, inclusion of aforementioned factors along with multi-factorial regression analysis would better clarify its role.
Journal Title: Journal of Surgical Oncology
Year Published: 2018
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!