Photo from wikipedia
Supermicorsurgical technique makes anastomosis of 0.3 to 0.8 mm lymphatics to subdermal veins possible. Identifying vascular access in lymphedema patients can be problematic sometimes as subcutaneous fat layer in lymphedema… Click to show full abstract
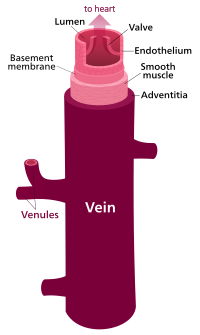
Supermicorsurgical technique makes anastomosis of 0.3 to 0.8 mm lymphatics to subdermal veins possible. Identifying vascular access in lymphedema patients can be problematic sometimes as subcutaneous fat layer in lymphedema patients is thickened and observation of veins through skin is difficult. A commonly associated problem is the absence of suitable veins in the proximity of a functional lymphatic vessel (fLV). Makoto et al. (2012) first described the use of a noncontact visualization system for identification of subcutaneous venules with a diameter of about 0.5–1.0 mm for LVA in a patient with bilateral lower limb lymphedema, with a resultant improvement in the surgical outcomes. We believe that not only their localization but also the absence of venous reflux determines the success of a LVA, as it is known, that venous pressure is usually higher than fLV pressure (Munn, 2015;Wardhan& Shelley, 2009), a reflux phenomenon of venous blood back into fLV is likely to occur after LVA with a vein with reflux. This can lead to a less long-term LVApatency rate, as described byYamamoto andKoshima (2014). We therefore now use a vein visualizer (VeinViewer Flex®, Christie Medical, USA), which is a non-contact vein visualization device as a preoperative standard diagnostic tool to produce a realtime digital mapping of veins and select free-reflux veins. To circumvent venous reflux a fast and easy method was applied to identify hidden valves and bifurcations that could potentially have an impact on the quality of LVA. After the preoperative subdermal injection of ICG, the VeinViewer was applied to target free-reflux vein near the fLV (Figure 1). Surgeons must be aware of the thrombosis risk after LVA and that it can be decreased by anticipating and preventing venous reflux into the lymphatic. We believe that the postoperative outcomes after LVA may be improved by preoperatively choosing the vein wisely.
Journal Title: Microsurgery
Year Published: 2018
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!