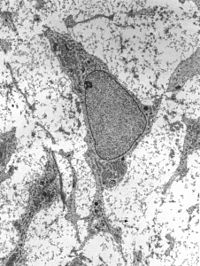
Photo from wikipedia
Mesenchymal stem cells (MSCs) are heterogeneous likely consisting of subpopulations with various therapeutic potentials. Here we attempted to acquire a subset of MSCs with enhanced effect in wound healing. We… Click to show full abstract
Mesenchymal stem cells (MSCs) are heterogeneous likely consisting of subpopulations with various therapeutic potentials. Here we attempted to acquire a subset of MSCs with enhanced effect in wound healing. We found that human placental MSCs expressing platelet-derived growth factor (PDGF) receptor (PDGFR)-β exhibited greater proliferation rates and generated more colony-forming unit-fibroblast (CFU-F), compared to PDGFR-β− MSCs. Notably, PDGFR-β+ MSCs expressed higher levels of pro-angiogenic factors such as Ang1, Ang2, VEGF, bFGF and PDGF. When 106 GFP-expressing MSCs were topically applied into excisional wounds in mice, PDGFR-β+ MSCs actively incorporated into the wound tissue, resulting in enhanced engraftment (3.92 ± 0.31 × 105 remained in wound by 7 days) and accelerated wound closure; meanwhile, PDGFR-β− MSCs tended to remain on the top of the wound bed with significantly fewer cells (2.46 ± 0.26 × 105) engrafted into the wound, suggesting enhanced chemotactic migration and engraftment of PDGFR-β+ MSCs into the wound. Real-Time PCR and immunostain analyses revealed that the expression of PDGF-B was upregulated after wounding; transwell migration assay showed that PDGFR-β+ MSCs migrated eightfold more than PDGFR-β− MSCs toward PDGF-BB. Intriguingly, PDGFR-β+ MSC-treated wounds showed significantly enhanced angiogenesis compared to PDGFR-β− MSC- or vehicle-treated wounds. Thus, our results indicate that PDGFR-β identifies a subset of MSCs with enhanced chemotactic migration to wound injury and effect in promoting angiogenesis and wound healing, implying a greater therapeutic potential for certain diseases.
Journal Title: Cellular and Molecular Life Sciences
Year Published: 2017
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!