Photo from wikipedia
We were pleased to read the response of Saithna and Jordan [14] to our recent article titled “Magnetic resonance arthrography is insufficiently accurate to diagnose biceps lesions prior to rotator… Click to show full abstract
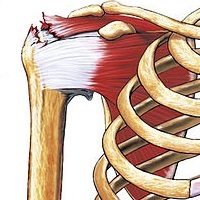
We were pleased to read the response of Saithna and Jordan [14] to our recent article titled “Magnetic resonance arthrography is insufficiently accurate to diagnose biceps lesions prior to rotator cuff repair” [10]. The authors made interesting remarks about the validity of arthroscopy for the diagnosis of biceps pathology, and supported our views that neither magnetic resonance imaging (including arthrography) nor clinical tests are sufficiently reliable in this context. First, Saithna and Jordan suspect that we might have miscited two of their works [9, 13] in our introduction, where they felt we “incorrectly suggested that [their] work supported the utility of Speed’s test”. We, therefore, verified our text and citations, and found that the first instance does not mention Speed’s test: “Recent studies [4, 11, 13], however, demonstrated limited accuracy of intra-operative arthroscopic assessment because of the non-visibility of the extra-articular portion of the LHB, a frequent lesion site”. It is true nonetheless that the second instance invokes the utility of Speed’s test, but later states its limited reliability: “Clinical tests, including the O’Brien [2, 12], Speed [2, 9] and hourglass [3] tests, as well as bicipital groove palpation [5], are all useful to some extent but none were proven to be accurate in confirming or ruling out biceps pathologies [3, 5, 6]”. We understand that our text could be misunderstood, but we thought that the remainder of the sentence clarifies our intended meaning. We realise, in retrospect, that we should have referred to the primary source Holtby et al. [7], rather than the secondary source of Jordan et al. [9]. Second, Saithna and Jordan emphasize “that arthroscopy should be considered an invalid gold standard, and that published figures for sensitivities and specificities of diagnostic modalities based upon arthroscopy are nugatory [9]”. While we agree that conventional arthroscopy is unreliable for the diagnosis of biceps tendinopathy and histopathologic abnormalities, for which open exploration is the current reference modality, our study used arthroscopy not only to diagnose tendinopathy, but also to inspect for biceps instabilities during various shoulder movements. Neither static imaging nor open exploration can reveal biceps tendon subluxations or dislocations that are best observed using dynamic ultrasound or arthroscopy. Therefore, while we agree that static arthroscopic findings are insufficiently robust to calculate sensitivity and specificity of MRA in general, we remain convinced that the dynamic arthroscopic tests we performed are the best tools available to assess biceps stability. Third, though our abstract did not mention intraand inter-observer agreements on MRA findings, we believe that our thorough comparison of anomalies seen by three independent observers (senior radiologist, senior surgeon, and junior surgeon) is a key strength of our study. The poor to fair agreement among observers confirms our take-home message that “MRA is insufficiently accurate to diagnose biceps lesions” regardless the gold standard. In our practice, to circumvent the absence of reliable clinical and radiographic tools to diagnose biceps pathology, we treat painful biceps that tested positive on O’Brien and Palm Up tests, or those with intraoperative pathological signs, by biceps tenodesis using interference screw fixation in the bicipital groove [1], which grants greater clinical improvements and success rates than soft tissue tenodesis This reply referes to the letter available at https ://doi.org/10.1007/ s0016 7-019-05698 -7.
Journal Title: Knee Surgery, Sports Traumatology, Arthroscopy
Year Published: 2019
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!