Photo from wikipedia
Sir, We have carefully read the interesting article by QuesadaGómez JM et al. [1] reviewing the clinical trials comparing calcifediol and cholecalciferol (vitamin D3) to address its relative efficacy to… Click to show full abstract
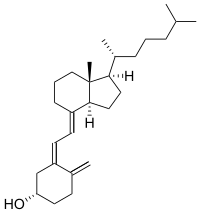
Sir, We have carefully read the interesting article by QuesadaGómez JM et al. [1] reviewing the clinical trials comparing calcifediol and cholecalciferol (vitamin D3) to address its relative efficacy to improve vitamin D status in terms of increasing serum 25-hidroxi-vitamin D (25OHD). As for the data from the paper, we conclude that the relative potency of calcifediol versus cholecalciferol ranges from 1.04 to 12 [1]. Therefore, in light of this evidence, it seems virtually impossible to ascertain the accurate equivalence between the two compounds in terms of international units (IU) of vitamin D. Historically, the biological activity of vitamin D compounds was compared on the basis of its anti-rachitic potency, and an IU was defined as the smallest biological potency to prevent rickets in rats, potency provided by the exact amount of 0.025 μg of cholecalciferol which was chosen as the gold standard vitamin D compound to quantify biological potency [2]. Probably, this election was made based on the fact that cholecalciferol is surely the most physiological form of vitamin D for its better availability in nature through intake of animal foods (mainly eggs and fish), and especially because cholecalciferol is endogenously synthesized in our skin during exposure to UVB (ultraviolet B) sunlight from 7dehydrocholesterol as vitamin D precursor [3]. This dose uncertainty can even have safety issues since we have clinical practice data of calcifediol used at intermittent doses of 266 μg × 2/month showing that 38% of patients could reach 25OHD levels above 60 ng/ml [4], which has been considered potentially harmful by IOM (Institute of Medicine) [5]. Apart from the question of this inaccuracy of calcifediol when dosing it in IU and considered that, according to guidelines, vitamin D must be dosed as biological potency in IU instead of μg [2, 3], we relevantly would like to state that we have carefully analyzed the scientific evidence of calcifediol and cholecalciferol on reduction of fracture risk in osteoporosis, and we conclude that, as long as we are aware, positive clinical trials have been performed only with cholecalciferol. Actually, we have identified one clinical trial with calcifediol by Peacock M et al., unfortunately, with negative results on fracture reduction [6]. Additionally, every phase III clinical trial of the most widely used anti-osteoporotic drugs has been performed supplementing patients with cholecalciferol as vitamin D form. So, if we intend to maximize the efficiency of these anti-osteoporotic drugs, we should use cholecalciferol as concomitant treatment [7, 8]. Therefore, because of accuracy in terms of dosing in IU and especially for better and stronger scientific evidence, our criteria concerning the Vitamin D form to supplement in osteoporosis is in agreement with the most relevant clinical guidelines including IOF (International Osteoporosis Foundation), which preferably recommend cholecalciferol (vitamin D3) [9–13], being calcifediol only to be considered in cases of severe hepatic insufficiency or intestinal malabsorption, as Quesada-Gomez JM et al. indeed suggest in their paper [1].
Journal Title: Osteoporosis International
Year Published: 2019
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!