Photo from wikipedia
To the Editor We read a recent publication by Bedada and Neerati on European Journal of Clinical Pharmacology with great interest, reporting the plasma concentrations of chlorzoxazone, an in vivo… Click to show full abstract
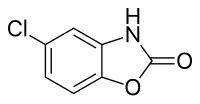
To the Editor We read a recent publication by Bedada and Neerati on European Journal of Clinical Pharmacology with great interest, reporting the plasma concentrations of chlorzoxazone, an in vivo CYP2E1 probe drug, being significantly increased after 10-days treatment of quercetin (500 mg twice daily) in healthy subjects [1]. Quercetin is a dietary flavonoid present in a wide variety of foods such as apples, berries, and onions and herbal products such as Ginkgo biloba extract and St. John’s Wort. Quercetin has received increasing attention because of its potential biological functions including anti-oxidation and antiinflammation [2], and thus to evaluate its potential to cause drug interactions is also an important issue. Through our literature search, we found that the authors recently reported the effect of quercetin on pharmacokinetics of diclofenac, a CYP2C9 probe drug, in healthy volunteers, using the same study design, i.e., subjects received 500 mg of quercetin twice daily for 10 days [3]. Surprisingly, quercetin treatment had a similar effect on pharmacokinetics of diclofenac (increased plasma concentrations by 1.8-fold) to those of chlorzoxazone [1]. We found that plasma concentration-time profiles of chlorzoxazone and diclofenac as well as the respective metabolites were almost identical in these two papers. In particular, it is pointed out that the metabolic ratio of chlorzoxazone and diclofenac was profoundly affected by quercetin as compared with previous CYP2C9or CYP2E-mediated herb-drug interaction studies [4]. There results suggest that short-term treatment with quercetin for 10 daysmay result in clinically relevant drug interactions, presumably by inhibiting CYP2E1 and CYP2C9. To determine whether we should accept these clinical findings, we briefly discuss possible mechanism underlying CYP2E1-mediated quercetin-chlorzoxazone interaction. Chlorzoxazone is a centrally acting muscle relaxant, and rapidly absorbed from the gastrointestinal tract [5]. CYP2E1, which is extensively expressed in the liver [6], plays a predominant role in chlorzoxazone metabolism. These suggest that, to increase chlorzoxazone systemic exposure, perpetrators would have to inhibit hepatic CYP2E1 activity. With respect to the inhibitory effects of quercetin on CYP2E1, Östlund et al. recently reported that quercetin slightly, but not physiologically relevant, inhibits CYP2E1 activity with Ki value of 52.1 μM in human liver microsomes [7]. In addition, Nguyen et al. reported that Cmax of quercetin following oral administration at a dose of 1500 mg was 8.9 μM after 1week pretreatment (500 mg three times daily) in humans [8]. Taken together with the fact that quercetin daily dose was 1000mg in the study by Bedada and Neerati, it seems unlikely that quercetin inhibited hepatic CYP2E1 and consequently increased plasma concentrations of chlorzoxazone. Involvement of other enzymes and transporters related to metabolism and disposition of chlorzoxazone may need to be considered. It is possible that the inhibition of efflux transporters such as P-glycoprotein and breast cancer resistance protein (BCRP) by quercetin may lead to elevate the plasma concentrations of their substrates [9, 10]. For instance, single pretreatment of high-dose curcumin (2 g) significantly elevated sulfasalazine systemic exposure by inhibiting intestinal BCRP in healthy volunteers [11]. To our knowledge, there are no reports investigating whether chlorzoxazone is a substrate of such efflux transporters; nevertheless, it cannot be ruled out that the enhanced AUC of chlorzoxazone could partly be attributed to the inhibition of efflux transport by quercetin. Clinical investigations on possible drug interactions with dietary supplements or herbs including quercetin are undoubtedly important. Both CYP2E1 and CYP2C9 play critical roles in hepatic metabolism of many drugs. Therefore, we hope that these findings will be verified in further studies. Electronic supplementary material The online version of this article (https://doi.org/10.1007/s00228-018-2479-4) contains supplementary material, which is available to authorized users.
Journal Title: European Journal of Clinical Pharmacology
Year Published: 2018
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!