Photo from wikipedia
Being physician or medical student is a complex task that became currently more subtle and difficult. On March 11, 2020 the World Health Organization (WHO) declared the global pandemic with… Click to show full abstract
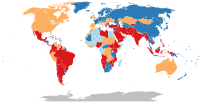
Being physician or medical student is a complex task that became currently more subtle and difficult. On March 11, 2020 the World Health Organization (WHO) declared the global pandemic with the occurrence and spread of a potentially life-threatening virus named COVID-19 with over 100.000 cases in 100 different countries affected by that time [1]. The pandemic spread fast and at the time when this paper goes in print over one million humans died as a result of viral action or related complications and over 36 million were infected [2]. The need to control the spread of the virus imposed in many countries measures of confinement, lockdown and social distancing. The orthopaedic practice was deeply affected by the pandemic and all the work schedules were altered. Guidelines from professional associations [3, 4, 5] proposed to postpone elective surgeries depending on the local situations and resources. The pandemic demonstrated the health system inequalities throughout the world, red lights turned on in many countries making visible how hard is to address such a global threat even in the twenty-first century. The pandemic changed the world, in all aspects, but we don’t know yet if for better or for worse. We are still far from the end of it. Dealing with the “new normal” is a stressful change, still a working process to all of us [6]. The teaching / learning, to all ages and grades and types of schools is altered in terms of methods, outcomes and results, learning could be affected with online classes, especially in the young age group of children and adolescents. The medical school students were affected too. In many countries the theoretical part activities shifted to online in the preclinical years [7, 8]. New sophisticated tools are developed to measure the efficacy of the e-learning. The side effects could be compensated in the following school year if normality equals again physical participation in class and school activities. Limitations on the clinical environment impacts classes, case discussions, lectures, internships and clinical rotations [8], as a result entire groups of students missed months of educational experiences, fundamental to their training as doctors. Authors also recognize that emergency remote teaching may not contain all the best practices in effective online instructions [9, 10]. As the medical education environment is cross-generational [11] consequences in the long term in the process and career trajectory of this new generation of doctors will have to be evaluated. The advance in technology and communication achieved in these lasts months is substantial and pointed out the qualities of the virtual learning, many activities are now easier, accessible and faster and eventually this will show us that not all the traditional classes and lectures are compulsory in the medical curriculum. The Covid-19 pandemic pushed the orthopaedic surgeon to integrate technology to help in many activities. Web-based meetings, daily / weekly meetings were the way to keep us connected, inside departments and among institutions. New platforms are now our work methods. In the * Marius M. Scarlat [email protected]
Journal Title: International Orthopaedics
Year Published: 2020
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!