Photo from wikipedia
Dear Editor, Thiamine deficiency is an under-recognized complication of allogeneic stem cell transplantation (allo-SCT). Thiamine plays a key role in cerebral energy utilization. Severe deficiency causes neuronal injury, sometimes leading… Click to show full abstract
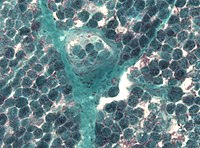
Dear Editor, Thiamine deficiency is an under-recognized complication of allogeneic stem cell transplantation (allo-SCT). Thiamine plays a key role in cerebral energy utilization. Severe deficiency causes neuronal injury, sometimes leading to Wernicke’s Encephalopathy (WE) [1–4]. One prospective study of 180 patients whose brains were autopsied after SCT showed that 5.55% of these patients had neuropathologic findings of WE [5]. The potential for significant neurologic complications warrants early detection of thiamine deficiency in this population. In this study, we present the long-term follow-up of allo-SCT patients from the Mount Sinai Hospital who were found to have low thiamine levels. We reviewed charts of all patients at the Mount Sinai Hospital who underwent allo-SCT between January 2014 and December 2016 (n = 135). Thiamine levels were checked when deemed appropriate by the treating teams. Deficiency was defined as thiamine diphosphate (TDP) level of < 70 nmol/L. Chart reviews identified patients’ primary diagnoses, transplant characteristics, symptoms of neurotoxicity, and radiography. Thirty-three patients had either whole blood or plasma thiamine levels checked. Of those, 10 had true thiamine deficiency. All 10 patients were female. Six had acute myeloid leukemia as the indication for their transplant. Six received grafts from 10/10 matched related (n = 3) or unrelated (n = 3) donors. Deficiency was discovered at a median of 91.5 days from transplant. Five demonstrated evidence of neurotoxicity: one had ocular disturbances attributed to WE, with signs of multifocal leukoencephalopathy found on MRI of the brain, while the neurologic symptoms of the four others were explained otherwise (Fig. 1). Five patients were taking systemic corticosteroids for active lower gastrointestinal (GI) tract GVHD and five patients were taking tacrolimus. One patient was receiving total parenteral nutrition (TPN). The cytotoxic conditioning regimens required prior to hematopoietic stem cell transplant commonly lead to prolonged neutropenia, mucositis, nausea, vomiting, and diarrhea. In addition, acute and chronic GVHD occurs in an estimated 45% [6] and 70% [7] of these patients, respectively, reducing oral intake and diminishing nutrient absorption. Comorbid renal dysfunction further reduces thiamine absorption by decreasing expression of vitamin transporters in the intestine, heart, liver, and brain [8]. Compounding this is the finding that energy requirements in the post-transplant period increase by 30– 50% [9]. Patients who experience subsequent malnutrition and malabsorption often require prolonged TPN to support
Journal Title: Annals of Hematology
Year Published: 2018
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!