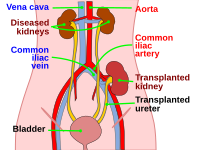
Photo from wikipedia
1. Post-transplant significant proteinuria is frequently caused by graft glomerular diseases including recurrent or de novo glomerulonephritis or antibody-mediated rejection (ABMR) [1–4]. The most common causes of posttransplant proteinuria are… Click to show full abstract
1. Post-transplant significant proteinuria is frequently caused by graft glomerular diseases including recurrent or de novo glomerulonephritis or antibody-mediated rejection (ABMR) [1–4]. The most common causes of posttransplant proteinuria are summarized in Table 1. 2. The light and immunofluorescence findings in the renal allograft biopsy demonstrated a membranous nephropathy (MN) with diffuse thickening of glomerular basement membrane (GBM) and diffuse granular C4d staining on the GBM. Electron microscopy findings, including thickening of GBM and subepithelial electron-dense deposits supported the diagnosis ofMN. C4d positivity was only detected along GBM and not along the peritubular capillary. C4d negative antibody-mediated rejection (ABMR) could not be ruled out due to the presence of moderate glomerulitis and mild peritubular capillaritis. In addition, the presence of tubulitis and interstitial infiltration suggested a T cellmediated rejection (Grade 1a). Native kidney biopsy findings at the age of 5 years were compatible with membranoproliferative glomerulonephritis, but not with MN. Therefore, the patient was diagnosed as de novo MN. 3. The etiology of de novo MN is still uncertain [5]. Recent findings in idiopathic MN show the importance of autoantibodies against the phospholipase A2 receptor (PLA2R). De novo MN is not typically associated either with circulating autoantibodies to the PLA2R or with positive tissue staining for the PLA2R antigen within immune deposits [6]. In the present case, anti-PLA2R was negative. Membranous nephropathy may usually be secondary, associated with infections, systemic lupus erythematosus, andmalignancies [7]. In our patient, serology for hepatitis B and C was negative. Serum complement levels, both C3 and C4 were within normal range. Antinuclear antibody was negative and anti-double-stranded DNAwas normal. There were no signs of other systemic diseases or malignancies. De novo MNmay also be associatedwith chronic and/or acute ABMR [1, 2]. Our patient had both C4d negative ABMR and T cell-mediated rejection features in the allograft biopsy. The patient had high titers of antibodies towards HLA Class 2, especially HLA-DQ. However, HLA tissue typing of the donor was not known, therefore the antibodies were not specified as Bdonor-specific antibody.^ Taken together, the most likely diagnosis of the patient was de novo MN associated with the rejection, especially with ABMR. 4. Due to significant proteinuria and loss of graft function in this patient with MNwith strong suspicion of ABMR, the patient was treated with plasma exchange, intravenous immunoglobulin and 3 doses of rituximab (375 mg/m). In addition, pulse steroids were given for the treatment of T cell-mediated rejection. Maintenance therapy included prednisolone, mycophenolate mofetil and tacrolimus with the increase in trough levels. Strict blood pressure control was achieved with ACE inhibition. HLA Class 2 antibodies decreased to 29%. After 14 months of the treatment, the patient is still being followed up in a good condition with a serum creatinine level of 1.1 mg/dL without proteinuria. This refers to the article that can be found at https://doi.org/10.1007/ s00467-019-04262-2.
Journal Title: Pediatric Nephrology
Year Published: 2019
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!