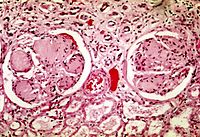
Photo from wikipedia
AimsTo determine the prevalence of diabetic nephropathy (DN) and non-diabetic renal disease (NDRD) in patients with type 2 diabetes mellitus (T2DM), and the important clinical predictors of renal outcome and… Click to show full abstract
AimsTo determine the prevalence of diabetic nephropathy (DN) and non-diabetic renal disease (NDRD) in patients with type 2 diabetes mellitus (T2DM), and the important clinical predictors of renal outcome and clinical course.MethodsWe conducted a retrospective analysis of clinical, laboratory, and histopathologic data from T2DM patients with renal involvement confirmed by renal biopsy (n = 505). The outcome was defined as the progression to end-stage renal disease (ESRD).ResultsRenal biopsy revealed that 302 patients (59.8%) had DN, 174 (34.5%) had NDRD, and 29 (5.7%) had NDRD superimposed on DN. In multivariate analysis, the absence of diabetic retinopathy (DR) (odds ratio (OR) 4.171, 95% confidence interval (CI) 1.810–9.612; P = 0.001), absence of hypertension (OR 2.412, 95% CI 1.095–5.315; P = 0.029), shorter duration of diabetes (OR 1.015, 95% CI 1.008–1.022; P < 0.001), lower-risk chronic kidney disease (CKD) heat map category (green, yellow and orange) (OR 3.885, 95% CI 1.289–11.707; P = 0.016) and lower glycated hemoglobin (HbA1c) (OR 1.339, 95% CI 1.114–1.610; P = 0.002) were significant clinical predictors of NDRD. Patients with DN had a poorer 5-year renal outcome than those with NDRD, and multivariate analysis identified DN as an independent risk factor for progression to ESRD, when adjusted for important clinical variables (P < 0.05).ConclusionsThis study has identified the absence of DR and hypertension, lower-risk CKD heat map category, shorter duration of diabetes, and lower HbA1c as useful clinical predictors of NDRD. Renal biopsy is recommended for patients with T2DM and renal disease to obtain an accurate diagnosis and determine timely disease-specific treatment, which should increase the chance of a good renal outcome.
Journal Title: Acta Diabetologica
Year Published: 2019
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!