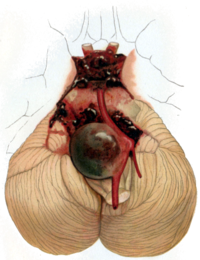
Photo from wikipedia
Background Previous studies have not evaluated the impact of illness severity and postrupture procedures in the cost of care for intracranial aneurysms. We hypothesize that the severity of aneurysm rupture… Click to show full abstract
Background Previous studies have not evaluated the impact of illness severity and postrupture procedures in the cost of care for intracranial aneurysms. We hypothesize that the severity of aneurysm rupture and the aggressiveness of postrupture interventions play a role in cost. Methods The Value Driven Outcomes database was used to assess direct patient cost during the treatment of ruptured intracranial aneurysm with clipping, coiling, and Pipeline flow diverters. Results One hundred ninety-eight patients (mean age 52.8 ± 14.1 years; 40.0% male) underwent craniotomy (64.6%), coiling (26.7%), or flow diversion (8.6%). Coiling was 1.4× more expensive than clipping ( p = .005) and flow diversion was 1.7× more expensive than clipping ( p < .001). More severe illness as measured by American Society of Anesthesia, Hunt/Hess, and Fisher scales incurred higher costs than less severe illness ( p < .05). Use of a lumbar drain protocol to reduce subarachnoid hemorrhage and use of an external ventricular drain to manage intracranial pressure were associated with reduced ( p = .05) and increased ( p < .001) total costs, respectively. Patients with severe vasospasm ( p < .005), those that received shunts ( p < .001), and those who had complications ( p < .001) had higher costs. Multivariate analysis showed that procedure type, length of stay, number of angiograms, vasospasm severity, disposition, and year of treatment were independent predictors of cost. Conclusions These results show for the first time that disease and vasospasm severity and intensity of treatment directly impact the cost of care for patients with aneurysms in the USA. Strategies to alter these variables may prove important for cost reduction.
Journal Title: Acta Neurochirurgica
Year Published: 2019
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!