Photo from wikipedia
Dear Editor, Pain is a rather frequent and highly disabling non-motor symptom of Parkinson’s disease (PD). In advanced PD patients, pain frequently occurs or is aggravated by the “off” condition… Click to show full abstract
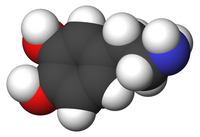
Dear Editor, Pain is a rather frequent and highly disabling non-motor symptom of Parkinson’s disease (PD). In advanced PD patients, pain frequently occurs or is aggravated by the “off” condition and may benefit by dopamine replacement therapy [1]. Rare cases, however, experience pain exacerbation as the consequence of involuntary movements during the “on” condition of along diphasic dyskinesia [1]. In these latter cases, opiates or other analgesics may help, despite the risk of cognitive/neuropsychiatric adverse events. Alternatively, pain management imposes reduction of dopaminergic therapy, in turn worsening fluctuations as the consequence of extreme narrowing of the therapeutic window to levodopa [1]. Levodopa/carbidopa intestinal gel (LCIG) ensures stabilization of plasma levodopa concentrations, thus limiting the presence and severity of fluctuations and involuntary movements, optimizing the risk/benefit ratio of levodopa administration, and ameliorating functioning and quality of life in advanced PD patients [2]. We report here the case of a patients presenting with disabling levodopa-related rightlimb dystonia who experienced significant reduction of pain and disability after switching to LCIG. A 77-year-old female, with positive family history for neurodegenerative disorders, diagnosed with idiopathic PD since 2004 and receiving dopamine replacement therapy since 2005, reported the development of levodopa-related fluctuations since 2010, and peak-dose dyskinesia and dystonia of the right leg since 2013. Due to the severity and progressive worsening of involuntary movements, with involvement of right arm and leg and profound negative impact on quality of life, she was forced to reduction of dopamine replacement therapy. Since 2019, therefore, she was treated with levodopa/benserazide 50/12.5 mg, six daily doses (3-h interval), and opicapone 50 mg (levodopa-equivalentdaily-dose–LEDD = 450 mg). While under such therapy, she kept suffering from painful peak-dose dystonia (VAS score 8) lasting approximately 1 h after each levodopa dose, and severe “off” state lasting at least 40 min between each dose. Moreover, she had very poor quality of sleep (PDSS-2 score 37) due to pain and discomfort secondary to muscle cramps and inability to turn around in bed and move due to prolonged “off” state along most nighttime. Her modified Hoehn and Yahr (H&Y) score was 5, the MDS-UPDRS-III score in “off” was 77. Since fulfilling the “5–2-1” Delphi Criteria for considering switch to advanced therapy [3], our patient was proposed LCIG. She agreed with this option, provided a testtube phase evaluation. After admission to our University Hospital and withdrawal form opicapone, she underwent a 3-day LCIG testing period under the following infusion parameters: morning dose 5.0 ml (i.e., the amount for filling the nose-intestinal tube), continuous rate 1.2 ml/h (24 mg/h). Along this period, involuntary movements almost completely disappeared, and the patient reported marked reduction of pain severity (VAS score 4–5). After PEG-J positioning, the patient was discharged under 24-h LCIG treatment with 1.4 ml/h (28 mg/h) infusion rate. Morning dose was reduced to 3.0 ml in order to fill the PEG-J jejunal tube soon after cleansing. Two weeks later, based on the lack of dyskinesia and dystonia, infusion rate was further increased to 1.6 ml/h (32 mg/h) along daytime (07:00 AM–11:00 PM), and maintained at 1.4 ml/h along nighttime (LEDD 736 mg). At the 2-month follow-up visit, the patient was able to walk with assistance for short tracks (H&Y score 4), the VAS score lowered to 3 along the short periods of involuntary movements occurring soon after tube cleansing (once every 2 days) and mild “off” periods lasting 30–60 min in the afternoon and 2–3 h along nighttime. The PDSS-2 score * Francesco E. Pontieri [email protected]
Journal Title: Neurological Sciences
Year Published: 2022
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!