Photo from wikipedia
While the indications and benefits of pelvic lymph node dissection (PLND) in rectal cancer surgery remain controversial, there is little debate about the technical demands of the procedure [1–3]. The… Click to show full abstract
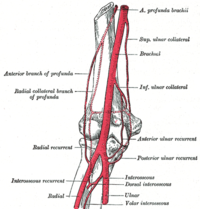
While the indications and benefits of pelvic lymph node dissection (PLND) in rectal cancer surgery remain controversial, there is little debate about the technical demands of the procedure [1–3]. The challenge of PLND arises from the (1) unfamiliarity of surgeons with the anatomy and procedure, (2) suboptimal dissection of planes often-times, especially in patients with gross lymphovascular disease and in those who have completed neoadjuvant radiotherapy, and (3) issues with operative field visualization and operator ergonomics. Our aim was to facilitate the understanding of the anatomy and planes of dissection in surgeons seeking to perform PLND. The key to appreciating the anatomy of the pelvic side wall (PSW) is to realize that dissection during PLND essentially converts the potential space of the PSW into a threedimensional (3D) compartment. Even if preoperative imaging was studied or modeled, the relationships between PSW structures are partly altered by intraoperative retraction. We describe how one PSW essentially becomes two triangular pyramidal compartments, defined by three planes, during PLND. To provide an easily replicable and economical medium for instruction, we have created an origami model using A4 size paper to facilitate the visualization of the 3D PSW (Video 1). The three planes, from medial to lateral, are the ureterohypogastric nerve fascia plane (UHNF), the vesicohypogastric fascia plane (VHF), and the external-iliac-muscular plane (EIM) (Fig. 1). Structures located along the UHNF include the urinary bladder, ureter, hypogastric nerve, pelvic splanchnic nerves, and pelvic plexus (Fig. 2). After medialization of the ureter, the UHNF can be separated from the middle plane (VHF), thereby creating the medial compartment which is made up of the paravesical space and pararectal space. The structures that traverse this compartment include vessels that arise from the internal iliac artery—the superior and inferior vesical arteries, middle rectal artery, uterine and vaginal arteries and their accompanying veins. The middle plane (VHF) essentially contains the internal iliac artery, leading anteriorly to the umbilical artery and its obliterated portion (the medial umbilical ligament). The other branches are given off as the internal iliac artery and it courses deeper caudally. The third and most lateral plane of the PSW is made up of the external iliac vessels, the psoas muscle, and the obturator internus muscle (Fig. 3). Between these two planes lies the lateral compartment, through which the obturator nerve and vessels run towards the obturator foramen. The internal pudendal vessels also course from the internal iliac towards the obturator internus fascia, passing through Alcock’s canal to enter the perineum. After conceptualizing the three planes and two compartments as a 3D operative field, the next step in PLND is to define the boundaries of dissection (Video 2). The proximal boundary of dissection is where the ureter crosses the common iliac artery, just before its bifurcation into the internal and external iliac arteries. As the dissection progresses, the other proximal landmark is the bifurcation of the iliac veins, where the obturator nerve can be seen entering the PSW compartment. Distally, the vas deferens or round ligament marks the end of dissection. The external circumflex iliac vein also serves as a useful landmark at this level. At a deeper level, dissection needs to be extended to the obturator foramen to completely remove the obturator group of lymph nodes. Electronic supplementary material The online version of this article (https ://doi.org/10.1007/s1015 1-020-02184 -y) contains supplementary material, which is available to authorized users.
Journal Title: Techniques in Coloproctology
Year Published: 2020
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!