Photo from wikipedia
An 81-year-old male was initially evaluated in a local emergency department for a 6-week history of diarrhea. He had a history of coronary artery disease with remote coronary artery bypass… Click to show full abstract
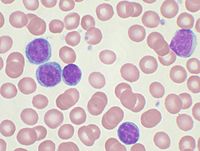
An 81-year-old male was initially evaluated in a local emergency department for a 6-week history of diarrhea. He had a history of coronary artery disease with remote coronary artery bypass graft and mechanical mitral valve placement, for which he was maintained on warfarin. He also had chronic obstructive pulmonary disease with chronic hypoxemic respiratory insufficiency for which he received continuous oxygen at a rate of 2 L/min. Prior to the onset of diarrhea, he had no chronic gastrointestinal (GI) symptoms. The diarrhea began acutely, was non-bloody, and eventually progressed to more than ten bowel movements daily. While he denied abdominal pain, fevers, chills, or nausea, he sustained a 10-pound weight loss during this time. There was no family history of inflammatory bowel disease. On presentation, his laboratory results included a white blood cell count of 28.0 × 103/μL (of which 44% were atypical lymphocytes), hemoglobin 12.1 g/dL, platelet count 146 × 103/μL, albumin 1.8 g/dL, erythrocyte sediment rate 15 mm/h (normal < 20), C-reactive protein 6.8 mg/dL (normal < 0.9), lactate dehydrogenase 734 U/L (normal < 340), and haptoglobin < 8 mg/dL. Clostridium difficile toxin stool antigen and stool cultures were negative. The remainder of his laboratory results were unremarkable. A computed tomography (CT) scan with intravenous contrast demonstrated significant inflammation and colonic wall thickening and possible narrowing of the rectosigmoid colon with surrounding fat stranding and significant retroperitoneal and mesenteric lymphadenopathy. There was also mesenteric vascular calcification with no vascular obstruction seen. There were no diverticula (Fig. 1). A colonoscopy showed severe inflammation of the rectosigmoid colon with edema and stenosis that could not be traversed. A diagnosis of possible Crohn’s disease was made based on endoscopic appearance, and he was transferred to our institution for further evaluation, treatment, and for consideration of initiation of anti-tumor necrosis factor (TNF) therapy. Upon transfer to our institution, he looked well with stable vital signs but had persistent diarrhea. He had no palpable lymphadenopathy. His laboratory evaluations were stable. We performed a flexible sigmoidoscopy that showed moderate mucosal inflammation, friability, and a few ulcerations, more pronounced in the sigmoid colon. There was no rectal sparing and no clear stricture (Fig. 2). Random biopsies showed a lamina propria expanded by small lymphocytes. Immunohistochemistry revealed the cell populations were cluster-of-differentiation (CD)20 dim, pairedbox containing (Pax)5, CD5, and B cell lymphoma (Bcl)2 positive, but CD10, Bcl1, Bcl6, terminal deoxynucleotidyl transferase (TdT), and lymphoid enhancer-binding factor 1 (LEF1) negative. The Ki67 proliferation index was low at less than 5%. Based on the mucosal appearance, histology, and tumor markers, a diagnosis of chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL)-related colitis was made (Fig. 3). Flow cytometry of peripheral blood showed a 47% kappa-restricted monotypic B cell population expressing CD19, with dim expression of CD5, CD20, CD22, CD23, and no expression of CD10 consistent with CLL/SLL. Fluorescence in situ hybridization showed a normal 46YX karyotype without rearrangements. After discussion of prognosis and comorbidities with the patient, he wished to pursue symptomatic support with a focus on palliative care and comfort. A trial of chlorambucil was initiated prior to discharge, with the main goal of improving * George Triadafilopoulos [email protected]
Journal Title: Digestive Diseases and Sciences
Year Published: 2018
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!