Photo from wikipedia
Chronic gastric-related conditions such as gastroparesis and functional dyspepsia are associated with significant qualityof-life impairment. Data derived from cross-sectional cohort samples suggest poor physicaland mentalhealth-related quality-of-life [1, 2], health-related costs… Click to show full abstract
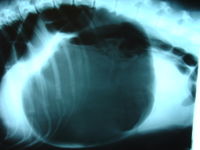
Chronic gastric-related conditions such as gastroparesis and functional dyspepsia are associated with significant qualityof-life impairment. Data derived from cross-sectional cohort samples suggest poor physicaland mentalhealth-related quality-of-life [1, 2], health-related costs (e.g., co-payments, medication costs) [3], and work impairment [2, 3]. Nevertheless, much of these data have been amassed from tertiary care center reports, including the NIH gastroparesis consortium [1, 4, 5]. Several studies have examined quality-of-life impairments in large community samples [6] and healthcare burdens in inpatient databases [7–9], but have been largely limited to gastroparesis samples. Thus, more data have been needed addressing the burdens engendered across the entire spectrum of gastric-related disorders among the broader population and across levels of care. In this issue of Digestive Disease and Sciences, Bielefeldt [10] describes trends in healthcare utilization and functional impairment based on data gathered by the Medical Expenditure Panel Survey (MEPS) collected between 2000 and 2015 that studied 10,699 individuals with gastric-related conditions. One area that has been largely unaddressed by prior research is the burden of gastric-related conditions outside of the tertiary care setting, since tertiary care patients may be more likely to have greater illness severity. Bielefeldt [10] addresses this issue by using the MEPS, a publicly available database of a US population-based survey of acute and chronic medical conditions, collected through in-person household interviews by the National Health Interview Survey. Using this large database, the author selected individuals who had self-reported “disorders of function of the stomach” (ICD-9 code 536) which includes the codes for achlorhydria, acute dilation of the stomach, persistent vomiting, gastroparesis, gastrostomy complications, dyspepsia and unspecified functional gastric disorder. Importantly, Bielefeldt [10] found that healthcare utilization related to the gastric condition was actually lower than the reference cohort (i.e., presumably all individuals in the database without ICD-9 code 536), and lower than many rates reported from tertiary care gastroparesis samples. While the group of individuals with gastric-related conditions in Bielefeldt [10] had a significantly greater average utilization of office visits, ambulatory visits, hospitalizations, and prescriptions than the reference cohort, patients did not attribute all of these visits to their gastric condition. This relatively lower frequency of visits attributed to the gastric condition was stable over the 16-year period. This is novel information, as healthcare utilization data have been either limited to tertiary center cohorts [2, 3] or to data only studying inpatient hospitalizations [7–9]. The time trends are also unique since they cut across levels of care, beyond time trends reported for inpatient hospitalizations related to gastroparesis [7–9]. Bielefeldt [10] also found that healthcare expenses and quality-of-life impairments were higher for those in the gastric-related condition group, but these findings were more difficult to interpret, since they were not able to tease apart costs specifically attributable to the gastric-related condition. Though the findings from Bielefeldt [10] expand knowledge regarding the healthcare utilization and impact of gastric conditions, there are certain limitations to the findings that can inspire future research: (1) burdens differentiated by condition type, (2) care fragmentation, and (3) other areas of quality-of-life impairment. First, while helpful to have data that capture a broader group of individuals with gastricrelated conditions, it would be interesting to see differences in healthcare burden by type of condition. It is possible that * Helen Burton Murray [email protected]
Journal Title: Digestive Diseases and Sciences
Year Published: 2020
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!