Photo from wikipedia
An electrical impedance-based noninvasive respiratory volume monitor (RVM) accurately reports minute volume, tidal volume and respiratory rate. Here we used the RVM to quantify the occurrence of and evaluate the… Click to show full abstract
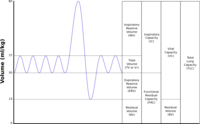
An electrical impedance-based noninvasive respiratory volume monitor (RVM) accurately reports minute volume, tidal volume and respiratory rate. Here we used the RVM to quantify the occurrence of and evaluate the ability of clinical factors to predict respiratory depression in the post-anesthesia care unit (PACU). RVM generated respiratory data were collected from spontaneously breathing patients following intraperitoneal surgeries under general anesthesia admitted to the PACU. Respiratory depression was defined as low minute ventilation episode (LMVe, < 40% predicted minute ventilation for at least 2 min). We evaluated for associations between clinical variables including minute ventilation prior to opioid administration and LMVe following the first PACU administration of opioid. Also assessed was a low respiratory rate (< 8 breaths per minute) as a proxy for LMVe. Of 107 patients, 38 (36%) had LMVe. Affected patients had greater intraoperative opioid dose, P = 0.05. PACU opioids were administered to 45 (42.1%) subjects, of which 27 (25.2%) had LMVe (P = 0.42) within 30 min following opioid. Pre-opioid minute ventilation < 70% of predicted normal value was associated with LMVe, P < 0.01, (sensitivity = 100%, specificity = 81%).Low respiratory rate was a poor predictor of LMVe (sensitivity = 11.8%). Other clinical variables (e.g., obstructive sleep apnea) were not found to be predictors of LMVe. Using RVM we identified that mild, clinically nondetectable, respiratory depression prior to opioid administration in the PACU was associated with the development of substantial subsequent respiratory depression during the PACU stay.
Journal Title: Journal of Clinical Monitoring and Computing
Year Published: 2017
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!