Photo from wikipedia
In this issue of the Journal of Thrombosis and Thrombolysis, Dr. Chong and colleagues present a Bayesian network meta-analysis of 15 randomized controlled trials (RCTs) and 43,875 patients in which… Click to show full abstract
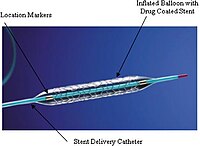
In this issue of the Journal of Thrombosis and Thrombolysis, Dr. Chong and colleagues present a Bayesian network meta-analysis of 15 randomized controlled trials (RCTs) and 43,875 patients in which different DAPT durations, e.g. short (1–3 months), intermediate (4–6 months) and standard (7–12 months), were stratified according to the two polymer categories, namely durable polymer (DP) or BP [3]. Whereas no differences were noticed across or within DAPT regimens regarding ischemic endpoints, including cardiac death, myocardial infarction (MI), target vessel revascularization, stroke and ST, BP-DES were surprisingly associated with a higher incidence of major bleeding. Indeed, not only the “standard DAPT” length of 7–12 months, but even the “intermediate” (4–6 months) and “short” (1–3 months) DAPT regimens, coupled with BP-DES, were associated with more bleeding as compared to short DAPT in the DP arm. Short DAPT with DP-DES (short-DP), noticeably, carried a more-than-halved risk of major bleeding compared to same-length DAPT with BP-DES (short-BP). Contrariwise, when examining the DP-DES results, only standard DAPT increased the risk of bleeding, whereas intermediate DAPT did not. Starting from highly complex statistical fundamentals, network meta-analyses allow synthetizing direct and indirect data to obtain multiple treatments comparisons. As such, they potentially fill important gaps in the knowledge and generate hypotheses for future research. Paradoxically, indirect comparisons might be considered of the highest interest, as, by definition, thay have not been previously investigated in head-to-head studies. On the other hand, conclusions exclusively derived by indirect comparisons In a seminal subanalysis of the Patient Related OuTcomes with Endeavor vs. Cypher stenting Trial (PROTECT) trial published in 2014, Camenzind and colleagues concluded that “the incidence of stent thrombosis [ST] in DES [drugeluting stent] trials should not be evaluated independently of DAPT [dual antiplatelet therapy] use, and the optimal duration of DAPT will likely depend upon stent type” [1]. It was, at the time, the most elegant demonstration that the long-term efficacy of coronary revascularization with DES could not be untwined from an optimal (e.g., durable) antiplatelet therapy. Since then, several technical innovations have helped cutting the risk of stent-related events, optimizing the bleeding-ischemia trade-off [2]. Among them, the introduction of biodegradable polymer (BP) (and, thereafter, of polymer-free) DES promised a major paradigm shift, due to the link between polymer-induced inflammation and late ST [2]. In this line of reasoning, early disappearance or wholesale avoidance of the “plastic” drug reservoir would mean taking the advantages of DES in the early phase and avoid their late drawbacks, potentially reducing the need for extended DAPT.
Journal Title: Journal of Thrombosis and Thrombolysis
Year Published: 2022
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!