Photo from wikipedia
An 87-year-old man presented with a 3-day history of epigastric pain associated with anorexia, nausea, and vomiting. He had presented with unexplored mild dysphagia for several months, along with a… Click to show full abstract
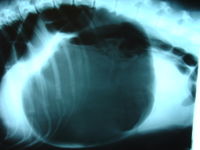
An 87-year-old man presented with a 3-day history of epigastric pain associated with anorexia, nausea, and vomiting. He had presented with unexplored mild dysphagia for several months, along with a maintained general condition. He had a medical history of asthma and atrial fibrillation, treated by acetylsalicylic acid and amiodarone. In the emergency room, he had no fever, and clinical examination revealed an abdominal distension with mild epigastric tenderness. Blood tests (i.e., complete blood count, serum electrolytes, C-reactive protein) were normal. The abdominal computed tomography (CT) showed a mesenteroaxial volvulus of the stomach (Fig. 1), revealed by a dilated stomach associated with a hernia of the pyloric antrum through the esophagus hiatus, mimicking a hiatal hernia. An oblique sagittal reconstruction showed a double beak sign, which corresponded to a crossing of the pyloric antrum and of the body of the stomach. There were no signs of gastric ischemia and no pneumoperitoneum. The gastric volvulus was surgically treated in emergency by laparoscopy, including the following steps: (i) exploration of the abdominal cavity in order to confirm the diagnosis and exclude both ischemia and gastric perforation (Fig. 2); (ii) cautious reduction of the volvulus; and (iii) esophageal hiatus closure and gastropexy. Postoperative course was uneventful with solid diet at day 1 and discharge at day 4. Gastric volvulus is a rare disease (the largest published series encompassed 36 patients over 14 years), occurring preferentially in the elderly patients. It consists of an abnormal rotation of the stomach, mainly along two potential axes: longitudinal (i.e., organoaxial volvulus) or transverse (i.e., mesenteroaxial volvulus). Although gastric volvulus can occur as a primary event (30%), it is usually secondary to other causes, mainly a paraesophageal hiatus hernia. Acute gastric strangulation may occur when rotation exceeds 180°: then, mortality can be as high as 30 to 50%. The clinical presentation of acute gastric volvulus is classically described as the Borchardt’s triad, which occurs in up to 70% of cases, and is composed of severe acute epigastric pain, vomiting then retching with the inability to vomit, and difficulty or inability to pass a nasogastric tube. However, the actual clinical presentation may be hardly specific, with a diagnosis only obtained by abdominal CT scan, whereas the risk of gastric ischemia is high and the necessity of surgical reduction, urgent. Moreover, most chronic incomplete gastric volvuli have nonspecific symptoms (e.g., pain, dysphagia, bloating, pyrosis) and remain unnoticed until the acute episode eventually occurs, as it happened in the present case. Since the mid 1990s, the laparoscopic approach has been proposed in this indication with good results: a 15% conversion rate and no major postoperative morbidity. In conclusion, acute gastric volvulus is a difficult and life-threatening diagnosis, which should be kept in mind in case of a nonspecific epigastric pain. Its surgical treatment, whether by laparoscopy on experienced hands or by open surgery, should be proposed in the emergency setting.
Journal Title: Journal of Gastrointestinal Surgery
Year Published: 2019
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!