Photo from wikipedia
A 34-year-old man with a history of epilepsy was found after falling into a washing tank, containing 60% cresol and 40% xylene in a plastic factory. He was brought to… Click to show full abstract
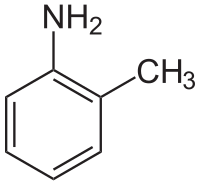
A 34-year-old man with a history of epilepsy was found after falling into a washing tank, containing 60% cresol and 40% xylene in a plastic factory. He was brought to a local hospital, where he presented as unconscious, in shock, and experiencing respiratory failure. Four hours post-exposure, he was given emergent endotracheal intubation and then transferred to a tertiary medical center. Upon arrival, he had altered mental status (Glasgow Coma Scale: E3VtM4). A physical examination revealed a brownish-black dermal discoloration over his torso, extremities, genital area, and buttocks, with a clear margin dividing the unaffected skin (Fig. 1, Panel A). The skin lesion was edematous and soft without bullae or eschar formation. Furthermore, the color of the urine in his urine drainage bag was dark red (Fig. 1, Panel B). Laboratory findings reported hemolysis, metabolic and respiratory acidosis, and acute renal failure. An ECG recording showed sinus tachycardia with multiple ventricular premature contractions. Diagnosed with 67% total body surface area (TBSA) of cresol chemical burning with systemic toxicity, he received decontamination treatment with large amounts of water and polyethylene glycol. He was then admitted to the intensive care unit with fluids and sodium bicarbonate supplement. After intensive care with venous-to-venous extracorporeal membrane oxygenation and continuous renal replacement therapy, he was discharged on the 45th day with a favorable outcome. The patient still had multiple skin scars. Cresol, a substituted phenol, is a commonly used disinfectant and has better antiseptic activity than phenol. Just like phenol, cresol shows great ability for skin penetration and causes severe dermal chemical burns. It functions as a caustic, causing different degrees of local tissue damage through cell wall disruption, protein denaturation, and coagulation necrosis [1]. In many cases, cresol ingestion may cause severe systemic toxicity, such as gastrointestinal corrosive injury, hemolysis, central nervous system and cardiovascular disturbances, respiratory distress, hepatotoxicity, and nephrotoxicity [1–3]. Compared to ingestion, severe systemic toxicity caused by skin absorption has rarely been reported in the literature. In fact, once significant amounts are absorbed, regardless of the method of exposure, such as inhalation, ingestion, dermal exposure, or parenteral administration, it can cause systemic toxicity [4]. The rate of cresol absorption through the skin is proportional to the size of the contact area and the duration of contact, rather than the concentration of the cresol solution [5]. We believe that our patient suffered severe systemic toxicity, including central nervous system depression, acute kidney damage, and acute respiratory distress syndrome that may have been the result of cresol exposure to large (67%) TBSA [4, 5]. Although the typical manifestation of black urine has only been reported previously in patients with intentional cresol ingestion [2, 3], the dark-colored urine of our patient demonstrated that cresol not only causes severe dermal burns but can also result in potentially fatal systemic toxicity within minutes to hours. Therefore, optimal management of cresol dermal exposure includes immediate skin decontamination with plenty of soapy water or polyethylene glycol and aggressive supportive care. * Yen-Chia Chen [email protected]
Journal Title: Internal and Emergency Medicine
Year Published: 2022
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!