Photo from wikipedia
Over the past decade, clinicians and researchers in the general critical care community have increasingly recognized and written about “post-intensive care syndrome,” or PICS. PICS refers to the physical, cognitive,… Click to show full abstract
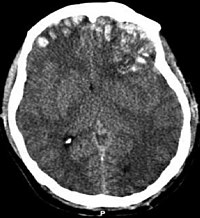
Over the past decade, clinicians and researchers in the general critical care community have increasingly recognized and written about “post-intensive care syndrome,” or PICS. PICS refers to the physical, cognitive, and/or psychiatric worsening of a patient following an admission to an intensive care unit (ICU) and the experience of being critically ill. A classic PICS scenario is the patient suffering from a lengthy ICU admission for severe adult respiratory distress syndrome (ARDS) and sepsis who makes a “full” recovery from their illness in the traditional sense, yet struggles with their energy levels, ability to return to work, and their mood for a prolonged period of time after discharge and rehabilitation. There has been increasing literature speculating on the multifactorial pathophysiology of post-ICU physical, cognitive, and mental decline; as well as teasing out what role prolonged exposure to the ICU environment itself may play into long-term psychiatric sequelae. However, the majority of studies and reviews regarding PICS have been published thus far by non-neurologists and non-neurointensivists. The reason for the neurocritical care community’s relative lack of participation in developing the concept of PICS is likely simple: The syndrome is challenging to define as an independent entity among a population of patients with primary brain or nervous system injury. Consider the myasthenic patient with prolonged weakness, the intracerebral hemorrhage (ICH) patient with permanent cognitive deficits, or the hemispheric stroke patient with long-term depression. Because of how these patients’ specific disorders inevitably drive their physical, cognitive, and mental disabilities far beyond ICU discharge, their situations are different from that of the recovering ARDS/sepsis patient without primary brain injury. Is it even helpful from either a clinical or research standpoint to label patients recovering from the neurocritical care illnesses above as suffering from “PICS?” Or does trying to discuss “PICS” among patients known to have primary neurological injury just generate confusion? The review article by LaBuzetta et al. attempts to tackle the question of how best to discuss and approach PICS within the neuroscience ICU [1]. For those readers who may be new to the concept of PICS, the review summarizes existing work in the non-neurological literature characterizing the syndrome among patients admitted without primary brain injury. Understanding that much of the focus of neurocritical care studies is already on functional outcomes, LaBuzetta et al. dedicate an important portion of their review to surveying what is known about cognitive and psychological outcomes among survivors of neurologic diseases such as ischemic stroke, ICH, subarachnoid hemorrhage, and traumatic brain injury. The challenges of implementing strategies to improve long-term physical, cognitive, and mental well-being in the neuroscience ICU—challenges such as minimizing continuous sedation in scenarios where some sedation is nevertheless needed, obtaining frequent neurological examinations in patients who nevertheless need sleep, and mobilizing patients despite their severe disability—are all acknowledged. The authors close their review with thoughts on how the neurocritical care community can be more involved in the study of PICS moving forward. Among their suggestions, one clear opportunity is for neurointensivists to not just walk away when a head computed tomography comes back negative but to play a larger role in *Correspondence: [email protected] Division of Neurocritical Care and Emergency Neurology, Center for Neuroepidemiology and Clinical Neurological Research, Yale School of Medicine, P.O. Box 208018, New Haven, CT 06520, USA
Journal Title: Neurocritical Care
Year Published: 2019
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!