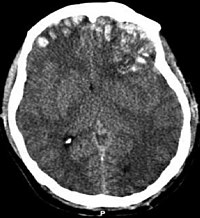
Photo from wikipedia
Pediatric neurocritical care survivorship is frequently accompanied by functional impairments. Lack of prognostic biomarkers is a barrier to early identification and management of impairment. We explored the association between blood… Click to show full abstract
Pediatric neurocritical care survivorship is frequently accompanied by functional impairments. Lack of prognostic biomarkers is a barrier to early identification and management of impairment. We explored the association between blood biomarkers and functional impairment in children with acute acquired brain injury. This study is a secondary analysis of a randomized control trial evaluating early versus usual care rehabilitation in the pediatric intensive care unit (PICU). Forty-four children (17 [39%] female, median age 11 [interquartile range 6–13] years) with acute acquired brain injury admitted to the PICU were studied. A single center obtained serum samples on admission days 0, 1, 3, 5, and the day closest to hospital discharge. Biomarkers relevant to brain injury (neuron specific enolase [NSE], S100b), inflammation (interleukin [IL-6], C-reactive protein), and regeneration (brain-derived neurotrophic factor [BDNF], vascular endothelial growth factor [VEGF]) were collected. Biomarkers were analyzed using a Luminex® bioassay. Functional status scale (FSS) scores were abstracted from the medical record. New functional impairment was defined as a (worse) FSS score at hospital discharge compared to pre-PICU (baseline). Individual biomarker fluorescence index (FI) values for each sample collection day were correlated with new functional impairment using Spearman rank correlation coefficient (ρ). Trends in repeated measures of biomarker FI over time were explored graphically, and the association between repeated measures of biomarker FI and new functional impairment was analyzed using covariate adjusted linear mixed-effect models. Functional impairment was inversely correlated with markers of regeneration and plasticity including BDNF at day 3 (ρ = − 0.404, p = .015), day 5 (ρ = − 0.549, p = 0.005) and hospital discharge (ρ = − 0.420, p = 0.026) and VEGF at day 1 (ρ = − 0.282, p = 0.008) and hospital discharge (ρ = − 0.378, p = 0.047), such that lower levels of both markers at each time point were associated with greater impairment. Similarly, repeated measures of BDNF and VEGF were inversely correlated with new functional impairment (B = − 0.001, p = 0.001 and B = − 0.001, p = 0.003, respectively). NSE, a biomarker of acute brain injury, showed a positive correlation between day 0 levels and new functional impairment (ρ = 0.320, p = 0.044). Blood-based biomarkers of regeneration and plasticity may hold prognostic utility for functional impairment among pediatric patients with neurocritical illness and warrant further investigation.
Journal Title: Neurocritical Care
Year Published: 2021
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!