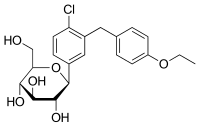
Photo from wikipedia
Introduction Based on post-marketing surveillance, concern has been raised that sodium–glucose cotransporter 2 inhibitors (SGLT2i) may increase the risk of necrotizing fasciitis of the perineum (Fournier’s gangrene, FG). As a result… Click to show full abstract
Introduction Based on post-marketing surveillance, concern has been raised that sodium–glucose cotransporter 2 inhibitors (SGLT2i) may increase the risk of necrotizing fasciitis of the perineum (Fournier’s gangrene, FG). As a result of the low incidence of FG, data from clinical trials may be insufficient to robustly assess this issue because of the relatively limited numbers of participants. Real-world evidence may help clarify the association between SGLT2i and FG in the type 2 diabetes (T2D) population. Methods A nested case–control study was performed using Truven Health MarketScan™ databases. Each patient with T2D hospitalized for FG between 1 April 2013 (when the first SGLT2i was available) and 31 March 2018 (latest available data) was matched (on the basis of sex, age, and cohort entry date) with six controls from the same cohort. The adjusted odds ratio (OR) of hospitalization for FG was estimated for patients receiving SGLT2i compared with those receiving two or more non-SGLT2i antihyperglycemic agents (AHAs) or insulin alone using conditional logistic regression. Results The cohort included 1,897,935 patients, with 216 hospitalized for FG (incidence rate, 5.2 events per 100,000 person-years). Patients with FG ranged from 23 to 79 years of age; 201 (93.1%) were men. Among the 216 FG cases, 9 (4.2%) were current SGLT2i users; among the 1296 matched controls, 100 (7.7%) were current SGLT2i users. Approximately 93% of SGLT2i were used in combination. The adjusted OR of FG in patients treated with SGLT2i compared with patients treated with two or more non-SGLT2i AHAs or insulin alone was 0.55 [95% CI 0.25–1.18]. Conclusion The study did not find that treatment with SGLT2i, as compared with treatment with two or more non-SGLT2i AHAs or insulin alone, was statistically significantly associated with an increased risk of hospitalization for FG. Additional studies are needed to corroborate the findings.
Journal Title: Diabetes Therapy
Year Published: 2020
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!