Photo from wikipedia
Levodopa treatment remains the gold standard for Parkinson's disease, but shortcomings related to the pharmacological profile, notably, oral administration and the consequent occurrence of motor complications, have led to the… Click to show full abstract
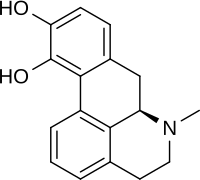
Levodopa treatment remains the gold standard for Parkinson's disease, but shortcomings related to the pharmacological profile, notably, oral administration and the consequent occurrence of motor complications, have led to the development of several add-on levodopa treatments or to research to improve the method of delivery. Motor fluctuations, and to a lesser extent non-motor fluctuations, concern half of the patients with Parkinson's disease after 5 years of disease and patients identified them as one of their most bothersome symptoms. Catechol-O-methyl transferase inhibitors (COMT-Is) are one of the recommended first-line levodopa add-on therapies for the amelioration of end-of dose motor fluctuations in patient with advanced Parkinson's disease. Currently, two peripheral COMT-Is are considered as first-line choices - entacapone (ENT), which was approved by the US Food and Drug Administration in 1999 and the European Committee in 1998; and opicapone (OPC), which was approved by the European Committee in 2016. A second-line COMT-I that requires regular hepatic monitoring, tolcapone (TOL), was approved by the Food and Drug Administration in 1998 and the European Committee in 1997. Of note, OPC also received Food and Drug Administration approval in 2021, but it is still only marketed in a few countries, including Germany, UK, Spain, Portugal, Italy, Japan, and USA, while ENT and TOL have a wider market. Our narrative review summarizes the pharmacokinetic/pharmacodynamic properties, clinical efficacy in terms of motor fluctuations, motor/non-motor symptoms, quality of life, and safety data of these three COMT-Is, as evidenced by randomized clinical trials, as well as by real-life observational studies. Overall, a phase III non-inferiority trial showed a similar effect between ENT and OPC on off-time (-60.8 min/day and -40.3 min/day, vs placebo, respectively), with a possible additional off-time reduction of 39 min/day, obtained when there is a switch from ENT to OPC. Concomitantly, TOL can reduce off-time by an average of 98 min/day. A significant though discrete concomitant reduction on the Unified Parkinson's Disease Rating Scale motor section (2-3 points) is obtained with all three drugs vs placebo. Data on quality of life are fewer and more heterogeneous, with positive results obtained especially in open-label studies. Effects on non-motor symptoms were investigated as secondary outcome only in a few studies, frequently by means of non-specific scales and a benefit was observed in open-label studies. Dopaminergic adverse effects were the most frequent, dyskinesia being the most common for the three drugs eventually requiring levodopa dose reductions. No urine discoloration and a very low incidence of diarrhea were found with OPC compared with ENT and TOL. Regular hepatic monitoring is needed only for TOL. A combination of COMT-Is with new formulations of levodopa, including the subcutaneous, intrajejunal, or new extended-release formulation, merits further exploration to improve the management of both mild and severe motor fluctuations.
Journal Title: CNS drugs
Year Published: 2022
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!