Photo from wikipedia
Hypogonadism and osteoporosis are frequently reported in HIV-infected men and, besides multifactorial pathogenesis, they might be directly linked because of testicular involvement in bone health. We evaluated the prevalence of… Click to show full abstract
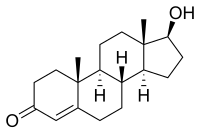
Hypogonadism and osteoporosis are frequently reported in HIV-infected men and, besides multifactorial pathogenesis, they might be directly linked because of testicular involvement in bone health. We evaluated the prevalence of osteoporosis and vertebral fractures (VFs) in HIV-infected men, and assessed their relationship with gonadal function. We enrolled 168 HIV-infected men (median age 53). Osteoporosis and osteopenia were defined with T-score ≤ – 2.5SD and T-score between – 1 and – 2.5SD, respectively. VFs were assessed by quantitative morphometric analysis. Total testosterone (TT), calculated free testosterone (cFT), Sex Hormone Binding Globulin (SHBG), Luteinizing Hormone (LH) and Follicle Stimulating Hormone (FSH) were obtained; overt hypogonadism was defined on symptoms and low TT or cFT, and classified into primary and secondary according to gonadotropins; compensated hypogonadism was defined as normal TT and cFT with high LH levels. Overall, osteoporosis and osteopenia were found in 87.5% of patients, and VFs were detected in 25% of them; hypogonadism was identified in 26.2% of cases. Osteoporotic patients had higher SHBG vs those with normal bone mineral density (BMD). Fractured patients were more frequently hypogonadal and with higher SHBG. SHBG showed negative correlation with both spine and femoral BMD, and positive correlation with VFs. In multivariate models, FSH showed negative impact only on femoral BMD, whereas older age and higher SHBG predicted VFs. We found a high burden of bone disease and hypogonadism in HIV-infected men, and we showed that the impact of gonadal function on bone health is more evident on VFs than on BMD.
Journal Title: Journal of Endocrinological Investigation
Year Published: 2021
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!