Photo from wikipedia
931 The relationship between histologicchorioamnionitis and biomarkers to identify neonates at increased risk of brain injury Ahizechukwu C. Eke, Frances Northington, Dhananjay Vaidya, Lavisha McClarin, Allen Everett, Ernest M. Graham… Click to show full abstract
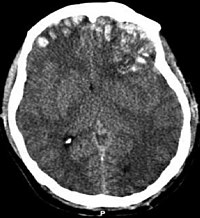
931 The relationship between histologicchorioamnionitis and biomarkers to identify neonates at increased risk of brain injury Ahizechukwu C. Eke, Frances Northington, Dhananjay Vaidya, Lavisha McClarin, Allen Everett, Ernest M. Graham Division of Maternal Fetal Medicine, Johns Hopkins University School of Medicine, Baltimore, MD, Division of Neonatology, Johns Hopkins University School of Medicine, Baltimore, MD, Dept of Internal Medicine & Biostatistics, Johns Hopkins University School of Medicine, Baltimore, MD, Division of Biostatistics, Johns Hopkins University School of Medicine, Baltimore, MD, Dept of Pediatrics, Johns Hopkins University School of Medicine, Baltimore, MD OBJECTIVE: Histologic chorioamnionitis has been linked to an increased risk of perinatal brain injury, possibly by direct cytotoxic effect or by increasing the susceptibility to hypoxia-ischemia. Glial Fibrillary Acidic Protein (GFAP) has been identified as a marker of perinatal brain injury in term and preterm neonates. Our hypothesis is that histologic chorioamnionitis may be linked with specific neonatal biomarker patterns that may be present even before the onset of clinical brain injury. STUDY DESIGN: This is a case-cohort study of all liveborn infants at 23-42 weeks of gestation admitted to the NICU from April 2009 to March 2016. Neonates with major congenital malformations and chromosomal abnormalities were excluded. Neonates were longitudinally evaluated for seven serum biomarkers GFAP, vascular growth factor (VEGF), brain-derived neurotrophic factor (BDNF), neurogranin (NRGN), IL-6, IL-8 and IL-10 on days 0 and 4 of life (table 1) in cord blood at delivery and from neonatal serum on day 4 of life. Multivariate marginal linear regression models and repeated measures analysis of variance (ANOVA) were used to investigate the relationship between biomarker levels and histologic chorioamnionitis, adjusting for gestational age, birth weight and mode of delivery. Statistical analysis was done using STATA 15. RESULTS: Of 1,810 pregnancies that met inclusion criteria, 536 (29.6%) were complicated by histologic chorioamnionitis. Gestational ages ranged from 23.3 to 41.3 (mean 29.3) weeks, and mean birthweight was 1203 ( 774) and 1293 ( 676) grams in cases and controls respectively. Mean GFAP levels were significantly higher at baseline (0.05 ng/mL in cases vs 0.02 ng/mL in controls; p1⁄40.048) and on day 4 of life (0.11 ng/mL in cases vs 0.00 ng/mL in controls; p1⁄4 0.004), table 1. Mean serum levels of BDNF and IL-6 were significantly lower at baseline in neonates born to mothers whose pregnancies were complicated by histologic chorioamnionitis compared to gestational age matched controls (p<0.05). CONCLUSION: Compared to gestational age matched controls, neonates of mothers with histologic chorioamnionitis had a significantly different pattern of blood biomarkers at delivery which persisted to day 4 of life and included elevated levels of GFAP. These changes in blood biomarker levels may aid in identification of neonates at increased risk of brain injury for early intervention prior to the development of clinical brain injury. Supported by NICHD R01HD086058.
Journal Title: American Journal of Obstetrics and Gynecology
Year Published: 2019
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!