Photo from wikipedia
BACKGROUND Women with refractory urgency urinary incontinence can be treated with onabotulinumtoxinA or sacral neuromodulation. Little data exists on the comparative effects of treatment of refractory UUI on other pelvic… Click to show full abstract
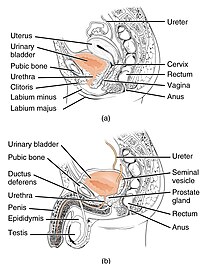
BACKGROUND Women with refractory urgency urinary incontinence can be treated with onabotulinumtoxinA or sacral neuromodulation. Little data exists on the comparative effects of treatment of refractory UUI on other pelvic floor complaints, such as bowel and sexual function. OBJECTIVE The objective of this study was to compare the impact of these treatments on fecal incontinence and sexual symptoms. METHODS This was a planned supplemental analysis of a randomized trial in women with refractory UUI treated with onabotulinumtoxinA (n=190) or sacral neuromodulation (n=174). Fecal Incontinence and sexual symptoms were assessed at baseline, 6, 12, and 24 months. Fecal incontinence symptoms were measured using the St Mark's (Vaizey) Fecal Incontinence severity scale. Sexual symptoms were measured using the Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire-12 (PISQ-12) and the Pelvic Organ Prolapse/Incontinence Sexual Questionnaire, IUGA-Revised (PISQ-IR). The PISQ-IR allows measurement of sexual symptoms in both sexually active and non-sexually active adults. Primary outcomes were change in Vaizey and PISQ-12 scores between baseline and 6 months. Secondary outcomes were change in PISQ-IR total and subscores between baseline and 6 months and change in Vaizey, PISQ-12 and PISQ-IR scores between baseline and 12 and 24 months. Intent to treat analysis was performed using repeated measures mixed model to estimate change in all parameters from baseline while adjusting for the baseline score. A subgroup analysis of women with clinically significant bowel symptoms was conducted based on baseline Vaizey score of ≥12. RESULTS At baseline, mean Vaizey scores were indicative of mild fecal incontinence symptoms and were not different between onabotulinumtoxinA and sacral neuromodulation groups (7.6+5.3 v 6.6+4.9, p=0.07). The proportion of sexually active women (56% v 63%, p=0.25), mean PISQ-12 score (33.4+7.5 v 32.7+6.7, p=0.55), or PISQ-IR subscores were also not different between the BTX and SNM groups at baseline. There was no difference between women treated with BTX and SNM at 6 months in improvement in fecal incontinence symptom score (Vaizey: -1.9, 95% CI -2.6 to -1.2 v -0.9, 95% CI -1.7 to -0.2, p=0.07) or sexual symptoms score (PISQ-12: 2.2, 95% CI 0.7 to 3.7 v 2.2, 95% CI 0.7 to 3.7, p=0.99). There was no difference in improvement between groups in the sexual symptom subscores in sexually active and non-sexually active women at 6 months. Similar findings were noted at 12 and 24 months. In a subgroup (onabotulinumtoxinA =33 and sacral neuromodulation =22) with clinically significant fecal incontinence at baseline (Vaizey score ≥12), there was a clinically meaningful improvement in symptoms in both groups from baseline to 6 months with no difference in improvement between the onabotulinumtoxinA and sacral neuromodulation groups (-5.1, 95% CI -7.3 to -2.8 v -5.6, 95% CI -8.5 to -2.6, p=0.8). CONCLUSIONS There were no differences in improvement of fecal incontinence and sexual symptoms in women with urgency urinary incontinence treated with onabotulinumtoxinA or sacral neuromodulation. Women with significant fecal incontinence symptoms at baseline had clinically important improvement in symptoms with no difference between the treatments. Our findings can help clinicians counseling women considering treatment for refractory urgency urinary incontinence.
Journal Title: American journal of obstetrics and gynecology
Year Published: 2019
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!