Photo from wikipedia
BACKGROUND Early pregnancy loss (EPL) is a common event in the first trimester, occurring in 15-20% of recognized pregnancies. A common evidence-based medical regimen for EPL management uses the prostaglandin… Click to show full abstract
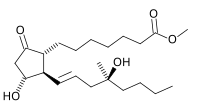
BACKGROUND Early pregnancy loss (EPL) is a common event in the first trimester, occurring in 15-20% of recognized pregnancies. A common evidence-based medical regimen for EPL management uses the prostaglandin E1 analogue misoprostol 800 mcg self-administered vaginally. The clinical utility of this regimen is limited by suboptimal effectiveness in women with a closed cervical os, with 29% of women with EPL requiring a second dose after three days, and 16% eventually requiring a uterine aspiration procedure. OBJECTIVES To evaluate characteristics associated with treatment success in women receiving medical management with mifepristone-misoprostol or misoprostol alone for early pregnancy loss (EPL). STUDY DESIGN We performed a planned secondary analysis of a randomized trial comparing mifepristone-misoprostol to misoprostol alone for EPL treatment. The published prediction model for success of single-dose vaginal misoprostol included the following variables: active bleeding, type of EPL (anembryonic pregnancy or embryonic/fetal demise), parity, gestational age, and treatment site; previous significant predictors were vaginal bleeding within the past 24 hours, and parity of 0 or 1 versus higher. We first assessed in bivariate analyses if these characteristics predicted differential proportions of women with success or failure; given the small proportion of treatment failures in the combined treatment arm, both arms were combined for analysis. We then performed a logistic regression analysis to assess the effect of these factors collectively in each of the two treatment groups separately as well as in the full cohort as a proxy for the combined treatment arm. We tested the ability of characteristics previously associated with misoprostol success to discriminate successful from failed treatment using receiver-operating characteristic curves. We calculated the area under the curve (AUC) to quantify the ability of the score to discriminate between treatment success or failure in each treatment arm as well as in the entire cohort. Using multivariable logistic regression, we then assessed our study population for other predictors of treatment success in both treatment groups, with and without mifepristone. RESULTS This analysis includes all 297 evaluable subjects in the primary study, including 148 in the mifepristone-misoprostol combined and 149 in the misoprostol-alone groups. Among women who had vaginal bleeding at the time of treatment, 15/17 (88%) in the mifepristone-misoprostol combined group and 12/17 (71%) of those in the misoprostol-alone group expelled the pregnancy. Among women with a parity of 0 or 1, 94/108 (87%) in the mifepristone-misoprostol combined group, and 66/95 (69%) of those in the misoprostol-alone group expelled the pregnancy. These clinical characteristics did not predict success above chance alone in the combined cohort (AUC=0.56, 95% CI 0.48-0.64). No other baseline clinical factors predicted treatment success in the misoprostol-alone or mifepristone pretreatment arms individually. In the full cohort, the only significant predictors of treatment success were mifepristone pretreatment (aOR 2.51, 95% CI 1.43-4.43), and smoking (aOR 2.15, 95% CI 1.03-4.49). CONCLUSION No baseline clinical factors predict success in women undergoing medical management of EPL with misoprostol. Adding mifepristone to the EPL medical management regimen improves treatment success and should be used regardless of baseline clinical characteristics.
Journal Title: American journal of obstetrics and gynecology
Year Published: 2020
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!